Abstract
Background: Patients who survive an acute myocardial infarction (MI) are at an increased risk of subsequent major cardiovascular events and (often sudden) cardiac death. The use of highly concentrated and purified omega-3 polyunsaturated fatty acids (n-3 PUFAs), in addition to standard secondary prevention after MI, results in a significant reduction in the risk of sudden death versus no n-3 PUFAs. This study assessed the cost effectiveness of adding n-3 PUFAs to the current secondary prevention treatment versus standard prevention alone after acute MI in five countries: Australia, Belgium, Canada, Germany and Poland.
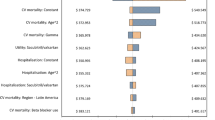
Methods: Based on the clinical outcomes of GISSI-P (Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico — Prevenzione) [MI, stroke, revascularisation rate and mortality], a decision model was built in DataPro™. The implications of adding n-3 PUFAs to standard treatment in patients aged 59 years with a recent history of MI were analysed from the healthcare payer’s perspective. The time horizon was 3.5 years (identical to GISSI-Prevenzione) but the effects on life expectancy through avoidance of cardiac events were calculated lifelong. Event costs were based on literature data. Life expectancy data for survivors of cardiac disease were taken from the Saskatchewan database and then adjusted by country. Results are expressed as extra cost (€) per life-year gained (LYG). Annual discounting of 5% was applied to health effects and costs.
Results: Treatment with highly concentrated n-3 PUFAs yielded between 0.261 (Poland) and 0.284 (Australia) LYG, at an additional cost of €787 (Canada) to €1439 (Belgium). The ICER varied between €2788 (Canada) and €5097 (Belgium) per LYG. Sensitivity analyses on effectiveness, cost of complications and discounting proved the robustness of the results. A second-order Monte Carlo simulation based on the 95% confidence intervals obtained from GISSI-P suggests that highly concentrated n-3 PUFAs are cost effective in 93% of simulations in Poland and in >98% of simulations in the other countries, assuming the country-specific societal willingness-to-pay threshold. Total costs were considerably increased by including healthcare costs incurred during the remaining life-years, but this had no impact on the ICER-based treatment recommendation.
Conclusions: Adding highly concentrated n-3 PUFAs to standard treatment in the secondary prevention of MI appears to be cost effective versus standard treatment alone in the five countries studied.







Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Braunwald E. Evolution of the management of acute myocardial infarction: a 20th century saga. Lancet 1998; 352: 1771–4
Capewell S, Livingston BM, MacIntyre K, et al. Trends in case-fatality in 117 718 patients admitted with acute myocardial infarction in Scotland. Eur Heart J 2000; 21: 1833–40
Haffner SM, Lehto S, Rtinnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998; 339: 229–34
Lampe FC, Whincup PH, Wannamethee SG, et al. The natural history of prevalent ischaemic heart disease in middle-aged men. Eur Heart J 2000; 21: 1052–62
de Lorgeril M, Salen P. Diet as preventive medicine in cardiology. Curr Opin Cardiol 2000; 15: 364–70
Huikuri HV, Castellanos A, Myetburg RJ. Sudden death due to cardiac arrhythmias. N Engl J Med 2001; 345: 1473–81
Myerburg RJ, Spooner PM. Opportunities for sudden death prevention: directions for new clinical and basic research. Cardiovasc Res 2001; 50: 177–85
Priori SG, AliotE, Blomstrom-Lundqvist C, et al. Task Force on Sudden Cardiac Death of the European Society of Cardiology. Eur Heart J 2001; 22: 1374–450
GISSI-Prevenzione Investigators. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 1999; 354: 447–55
Marchioli R, on behalf of the GISSI-Prevenzione Investigators. Treatment with n-3 polyunsaterated fatty acids after myocardial infarction: results of the GISSI-Prevenzione Trial. Eur Heart J Suppl 2001; 3 Suppl. D: D85–97
Franzosi MG, Brunetti M, Marchioli R, et al. Cost-effectiveness analysis of n-3 polyunsaturated fatty acids (PUFA) after myocardial infarction: results from Gruppo Italiano per 10 Studio della Sopravvivenza nell’Infarto (GISSI)-Prevenzione Trial. Pharmacoeconomics 2001; 19: 411–20
International Society of Pharmacoeconomics and OutcomesResearch [online]. Available from URL: http://wwwispor.org/PEguidelines/ [Accessed2005 Sep]
Organisation for Economic Co-operation and Development website [online]. Available from URL: http://www.oecd.p4.siteinternet.com/publications/doifiles/302006011PI-1O-01-04-t01.xls [Accessed 2006 Jan]
Economic Policy Committee 2001. Budgetary challenges posed by ageing populations: the impact on public spending on pensions, health and long-term care for the elderly and possible indicators of the long-term sustainability of public finances [online]. Available from URL: http://www.efrp.org/downloads/eu-publications/Budgetary_challenges.pdf [Accessed 2006 January]
Australian Government Department of Health and Ageing. Public sector estimated cost weights round 8 AR-DRG v5.0 [online]. Available from URL: http://www.health.gov.au/internet/wcms/publishing.nsf/Content/BB918453BBAB7AB0CA2570C1000230B0?.OpenDocument [Accessed 2006 Jan]
Grover SA, Coupal L, Zowall H, et al. How cost-effective is the treatment of dyslipidemia in patients with diabetes but without cardiovascular disease? Diabetes Care 2001; 24: 45–50
DRG Research group, Universitätsklinikum [online]. Available from URL: http://drg.uni-muenster.de/kodierung/kodierung.html [Accessed 2005 Sept]
Haldemann R, Luscher TF, Szucs ID. Cost effectiveness of clopidogrel in secondary cardiovascular prevention: a cost-effectiveness analysis based on the Caprie Study. Schweiz Rundsch Med Prax 2001 Mar 29; 90: 539–45
Lamotte M, Caekelbergh K, Annemans L, et al. Assessment of the cost of cardiovascular death [abstract]. Value Health 2003; 6: 658
Jones PJ, Lau VW. Effect of n-3 polyunsaturated fatty acids on risk reduction of sudden death. Nutr Rev 2002 Dec; 60 (12): 407–9
Statistics Canada. Canadian specific medical inflation index [online]. Available from URL: http://www40.statcan.ca/101/cstOl/econ150a.htm [Accessed 2006 Jan]
National Sickness Fund. Catalogue of Polish National Sickness Fund [Excel]. 2004
Annemans L, Lamotte M, Levy E, et al. Cost-effectiveness analysis of clopidogrel versus aspirin in patients with atherothrormosis based on the CAPRIE trial. J Med Econ 2003; 6: 55–68
Coy P, Schaafsma J, Schofield JA. The cost-effectiveness and cost-utility of high-dose palliative radiotherapy for advanced non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2000 Nov 1; 48 (4): 1025–33
Mauskopf JA, Cates SC, Griffin AD, et al. Cost effectiveness of zanamivir for the treatment of influenza in a high risk population in Australia. Pharmacoeconomics 2000; 17: 611–20
Abhyankar B. Further reduction in mortality following myocardial infarction. Hosp Med 2002; 63: 610–4
Euroaspire II Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries: principal results from Euroaspire II Euro Heart Survey Programme. Eur Heart J 2001; 22: 554–72
Christensen JH, Riahi S, Schmidt EB, et al. n-3 Fatty acids and ventricular arrhythmias in patients with ischaemic heart disease and implantable cardioverter defibrillators. Europace 2005; 7: 338–44
Brouwer IA, Zock PL, Wever EF, et al. Rationale and design of a randomised controlled clinical trial on supplemental intake of n-3 fatty acids and incidence of cardiac arrhythmia: SOFA. Eur J Clin Nutr 2003; 57: 1323–30
Mozaffarian D, Ascherio A, Hu FE, et al. Interplay between different polyunsaturated fatty acids and risk of coronary heart disease in men. Circulation 2005; 111: 157–64
Caro J, Klittich W, McGuire A, et al. The West of Scotland coronary prevention study: economic benefit analysis of primary prevention with pravastatin. BMJ 1997; 315: 1577–82
Pharoah PDP, Hollingworth W. Cost-effectiveness oflowering cholesterol concentration with statins in patients with and without pre-existing coronary heart disease: life table method applied to health authority population. BMJ 1996; 312: 1443–8
Tsevat J, Kuntz KM, Orav EJ, et al. Cost-effectiveness of pravastatin therapy for survivors of myocardial infarction with average cholesterol levels. Am Heart J 2001; 141: 727–34
Muls E, Van Ganse E, Closon MC. Cost-effectiveness of pravastatin in secondary prevention of coronary heart disease: comparison between Belgium and the United States of a projected risk model. Atherosclerosis 1998; 137 Suppl.: S111–6
Brown RE, Henderson RA, Koster D, et al. Cost effectiveness of eptifibatide in acute coronary syndromes: an economic analysis of Western European patients enrolled in the PURSUIT trial. The platelet IIa/IIb in unstable angina: receptor suppression using integrilin therapy. Eur Heart J 2002 Jan; 23 (1): 50–8
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lamotte, M., Annemans, L., Kawalec, P. et al. A Multi-Country Health Economic Evaluation of Highly Concentrated N-3 Polyunsaturated Fatty Acids in Secondary Prevention after Myocardial Infarction. Pharmacoeconomics 24, 783–795 (2006). https://doi.org/10.2165/00019053-200624080-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200624080-00005