Abstract
BACKGROUND: In ambulatory care settings, patients with limited English proficiency receive lower quality of care. Limited information is available describing outcomes for inpatients.
OBJECTIVE: To investigate the effect of English proficiency on length of stay (LOS) and in-hospital mortality.
DESIGN: Retrospective analysis of administrative data at 3 tertiary care teaching hospitals (University Health Network) in Toronto, Canada.
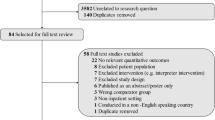
PARTICIPANTS: Consecutive inpatient admissions from April 1993 to December 1999 were analyzed for LOS differences first by looking at 23 medical and surgical conditions (59,547 records) and then by a meta-analysis of 220 case mix groups (189,119 records). We performed a similar analysis for in-hospital mortality.
MEASUREMENTS: LOS and odds of in-hospital death for limited English-proficient (LEP) patients relative to English-proficient (EP) patients.
RESULTS: LEP patients stayed in hospital longer for 7 of 23 conditions (unstable coronary syndromes and chest pain, coronary artery bypass grafting, stroke, craniotomy procedures, diabetes mellitus, major intestinal and rectal procedures, and elective hip replacement), with LOS differences ranging from approximately 0.7 to 4.3 days. A meta-analysis using all admission data demonstrated that LEP patients stayed 6% (approximately 0.5 days) longer overall than EP patients (95% confidence interval, 0.04 to 0.07). LEP patients were not at increased risk of in-hospital death (relative odds, 1.0; 95% confidence interval, 0.9 to 1.1).
CONCLUSIONS: Patients with limited English proficiency have longer hospital stays for some medical and surgical conditions. Limited English proficiency does not affect in-hospital mortality. The effect of communication barriers on outcomes of care in the inpatient setting requires further exploration, particularly for selected conditions in which length of stay is significantly prolonged.
Similar content being viewed by others
References
U.S. Census Bureau American FactFinder. Available at: http://factfinder.census.gov/servlet/BasicFactsServlet. Accessed April 30, 2002.
Fourth National Survey of Ethnic Minorities. Policy Studies Institute, Health Education Authority; 1992. United Kingdom.
Adapted from: Statistic’s Canada’s Internet Site. Available at: http://www.statcan.ca. Accessed May 3, 2001.
Fox SA, Stein JA. The effect of physician-patient communication on mammography utilization by different ethnic groups. Med Care. 1991;29:1065–82.
Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. J Gen Intern Med. 2000;15:256–64.
Tocher TM, Larson EB. Do physicians spend more time with non-English-speaking patients? J Gen Intern Med. 1999;14:303–9.
Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275:783–8.
Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103:1253–6.
Adapted from: Statistics Canada’s internet site. Available at: http://www.statcan.ca/english/Pgdb/popula.htm. Accessed July 3, 2001.
Pink GH, Bolley HB. Physicians in health care management: 4. Case Mix Groups and Resource Intensity Weights: physicians and hospital funding. CMAJ. 1994;150:1255–61.
Pink GH, Bolley HB. Physicians in health care management: 3. Case Mix Groups and Resource Intensity Weights: an overview for physicians. CMAJ. 1994;150:889–94.
Naglie G, Tansey C, Kirkland JL, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ. 2002;167:25–32.
Landis RJ, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Baker GR, Anderson GM, Brown AD, McKillop I, Montgomery C, Murray MA, Pink GH. The Hospital Report ’99. A balanced report card for Ontario acute care hospitals. Technical report. Available at: http://www.oha.com. Accessed March 21, 2000.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assessment: the Charlson comorbidity index. Methods Inf Med. 1993;32:382–7.
Rochon PA, Katz JN, Morrow LA, et al. Comorbid illness is associated with survival and length of hospital stay in patients with chronic disability. A prospective comparison of three comorbidity indices. Med Care. 1996;34:1093–101.
Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–10.
Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999;341:1359–67.
Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79:340–9.
Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–36.
Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Smith TC, Spiegelhalter DJ, Thomas A. Bayesian approaches to random-effects meta-analysis: a comparative study. Stat Med. 1995;14:2685–99.
Spiegelhalter DJ. Winbugs Version 1.2 User Manual; 1999. Cambridge, England: MRC Biostatistics Unit.
Sin DD, Tu JV. Are elderly patients with obstructive airway disease being prematurely discharged? Am J Respir Crit Care Med. 2000;161:1513–7.
Ramirez JA, Vargas S, Ritter GW, et al. Early switch from intravenous to oral antibiotics and early hospital discharge: a prospective observational study of 200 consecutive patients with community-acquired pneumonia. Arch Intern Med. 1999;159:2449–54.
Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269:1537–9.
Diehl AK, Westwick TJ, Badgett RG, Sugarek NJ, Todd KH. Clinical and sociocultural determinants of gallstone treatment. Am J Med Sci. 1993;305:383–6.
Perez-Stable EJ, Napoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997;35:1212–9.
Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14:409–17.
Shi L. Patient and hospital characteristics associated with average length of stay. Health Care Manage Rev. 1996;21:46–61.
Clarke A. Why are we trying to reduce length of stay? Evaluation of the costs and benefits of reducing time in hospital must start from the objectives that govern change. Qual Health Care. 1996;5:172–9.
Fine MJ, Pratt HM, Obrosky DS, et al. Relation between length of hospital stay and costs of care for patients with community-acquired pneumonia. Am J Med. 2000;109:378–85.
Author information
Authors and Affiliations
Corresponding author
Additional information
This research was supported by the University Health Network General Internal Medicine Clinical Research Fund. Ara John-Baptiste is supported by a Canada Graduate Scholarship from the Canadian Institutes of Health Research. Gary Naglie was partially supported by the Mary Trimmer Chair in Geriatric Medicine Research from the University of Toronto.
Rights and permissions
About this article
Cite this article
John-Baptiste, A., Naglie, G., Tomlinson, G. et al. The effect of English language proficiency on length of stay and in-hospital mortality. J GEN INTERN MED 19, 221–228 (2004). https://doi.org/10.1111/j.1525-1497.2004.21205.x
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2004.21205.x