Abstract
Objective:
Current scoring systems, which adjust prediction for severity of illness, do not account for higher observed mortality in neonatal intensive care units (NICUs) of children's hospitals than that of perinatal centers. We hypothesized that three potential predictors, (a) admission from another NICU, (b) presence of congenital anomalies and (c) need for surgery, would modify expected mortality and/or length of stay for infants admitted to NICUs in children's hospitals.
Study Design:
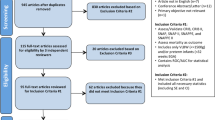
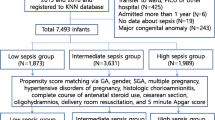
We reviewed consecutive admissions to two NICUs in children's hospitals in Canada. We performed regression analyses to evaluate these potential predictors and severity-of-illness indices for the outcomes of mortality and length of stay.
Result:
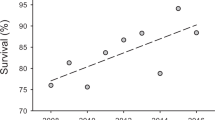
Of 625 neonatal admissions, transfer from another NICU, congenital anomalies requiring admission and surgery were identified in 371 (59%). Using logistic regression, mortality was predicted based on admission from another NICU (odds ratio (OR) 1.92; 95% confidence interval (CI) 1.04, 3.57), congenital anomalies (OR 7.28; 95% CI 3.69, 14.36) and a validated severity-of-illness score, the Score for Neonatal Acute Physiology Perinatal Extension Version II (SNAPPE-II; OR 1.07; 95% CI 1.05, 1.09 per point). By contrast, surgical intervention was predictive of survival (OR 0.35; 95% CI 0.18, 0.67). Length of stay ⩾21 days was predicted by SNAPPE-II (OR 1.02; 95% CI 1.01, 1.03 per point), congenital anomalies (OR 2.47; 95% CI 1.60, 3.79) and surgery (OR 2.73; 95% CI 1.77, 4.21).
Conclusion:
Fair performance comparisons of NICUs with different case-mixes, such as children's hospital and perinatal NICUs, in addition to severity-of-illness indices, should account for admissions from another NICU, congenital anomalies and surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Sankaran K, Chien LY, Walker R, Seshia M, Ohlsson A . Variations in mortality rates among Canadian neonatal intensive care units. CMAJ 2002; 166: 173–178.
Shah PS, Shah V, Qiu Z, Ohlsson A, Lee SK . Improved outcomes of outborn preterm infants if admitted to perinatal centers versus freestanding pediatric hospitals. J Pediatr 2005; 146: 626–631.
Lui K, Abdel-Latif ME, Allgood CL, Bajuk B, Oei J, Berry A et al. Improved outcomes of extremely premature outborn infants: effects of strategic changes in perinatal and retrieval services. Pediatrics 2006; 118: 2076–2083.
National Association of Children's Hospitals and Related Institutions. Child Health from the Nation's Children's Hospitals Trends Update. National Association of Children's Hospitals, 2007 [cited 2007 Jun 1]; available at http://www.childrenshospitals.net.
Spitz L, Wallis M, Graves HF . Transport of the surgical neonate. Arch Dis Child 1984; 59: 284–288.
Hackel A, Badgwell JM, Binding RR, Dahm LS, Dunbar BS, Fischer CG et al. Guidelines for the pediatric perioperative anesthesia environment. American Academy of Pediatrics. Section on Anesthesiology. Pediatrics 1999; 103: 512–515.
Stoodley N, Sharma A, Noblett H, James D . Influence of place of delivery on outcome in babies with gastroschisis. Arch Dis Child 1993; 68: 321–323.
Escarce JJ, Kelley MA . Admission source to the medical intensive care unit predicts hospital death independent of APACHE II score. JAMA 1990; 264: 2389–2394.
Dragsted L, Jorgensen J, Jensen NH, Bonsing E, Jacobsen E, Knaus WA et al. Interhospital comparisons of patient outcome from intensive care: importance of lead-time bias. Crit Care Med 1989; 17: 418–422.
Last JM . A Dictionary of Epidemiology. 2nd edn. Oxford University Press: New York, 1988.
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991; 100: 1619–1636.
Richardson DK, Tarnow-Mordi WO, Escobar GJ . Neonatal risk scoring systems. Can they predict mortality and morbidity? Clin Perinatol 1998; 25: 591–611.
The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. The International Neonatal Network. Lancet 1993; 342: 193–198.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK . SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 2001; 138: 92–100.
Richardson DK, Gray JE, McCormick MC, Workman K, Goldmann DA . Score for Neonatal Acute Physiology: a physiologic severity index for neonatal intensive care. Pediatrics 1993; 91: 617–623.
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Inpatient Perinatal Care Services. American Academy of Pediatrics: Elk Grove Village, IL, American College of Obstetricians and Gynecologists: Washington, DC 1997.
Harris TR, Isaman J, Giles HR . Improved neonatal survival through maternal transport. Obstet Gynecol 1978; 52: 294–300.
Cordero L, Backes CR, Zuspan FP . Very low-birth weight infant. I. Influence of place of birth on survival. Am J Obstet Gynecol 1982; 143: 533–537.
Lamont RF, Dunlop PD, Crowley P, Levene MI, Elder MG . Comparative mortality and morbidity of infants transferred in utero or postnatally. J Perinat Med 1983; 11: 200–203.
Kollee LA, Verloove-Vanhorick PP, Verwey RA, Brand R, Ruys JH . Maternal and neonatal transport: results of a national collaborative survey of preterm and very low birth weight infants in The Netherlands. Obstet Gynecol 1988; 72: 729–732.
Shlossman PA, Manley JS, Sciscione AC, Colmorgen GH . An analysis of neonatal morbidity and mortality in maternal (in utero) and neonatal transports at 24–34 weeks’ gestation. Am J Perinatol 1997; 14: 449–456.
Empana JP, Subtil D, Truffert P . In-hospital mortality of newborn infants born before 33 weeks of gestation depends on the initial level of neonatal care: the EPIPAGE study. Acta Paediatr 2003; 92: 346–351.
Harding JE, Morton SM . Adverse effects of neonatal transport between level III centres. J Paediatr Child Health 1993; 29: 146–149.
Towers CV, Bonebrake R, Padilla G, Rumney P . The effect of transport on the rate of severe intraventricular hemorrhage in very low birth weight infants. Obstet Gynecol 2000; 95: 291–295.
Yoder BA . Long distance perinatal transport. Am J Perinatol 1992; 9: 75–79.
Beeram M, Solarin K, Young M, Abedin M . Morbidity and mortality of infants born before arrival at the hospital. Clin Pediatr (Phila) 1995; 34: 313–316.
Lee TH, Torchiana DF, Lock JE . Is zero the ideal death rate? N Engl J Med 2007; 357: 111–113.
Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA . Accepting critically ill transfer patients: adverse effect on a referral center's outcome and benchmark measures. Ann Intern Med 2003; 138: 882–890.
Hudome SM, Kirby RS, Senner JW, Cunniff C . Contribution of genetic disorders to neonatal mortality in a regional intensive care setting. Am J Perinatol 1994; 11: 100–103.
Escobar GJ, Fischer A, Li DK, Kremers R, Armstrong MA . Score for neonatal acute physiology: validation in three Kaiser Permanente neonatal intensive care units. Pediatrics 1995; 96: 918–922.
Ling EW, Sosuan LC, Hall JC . Congenital anomalies: an increasingly important cause of mortality and workload in a neonatal intensive care unit. Am J Perinatol 1991; 8: 164–169.
Ling EW . Frequency and load of congenital anomalies in a neonatal intensive care unit, prenatal diagnosis, and perinatal management. Semin Perinatol 1992; 16: 352–357.
Van Regemorter N, Dodion J, Druart C, Hayez F, Vamos E, Flament-Durand J et al. Congenital malformations in 10 000 consecutive births in a university hospital: need for genetic counseling and prenatal diagnosis. J Pediatr 1984; 104: 386–390.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest: The authors state no conflict of interest.
Rights and permissions
About this article
Cite this article
Berry, M., Shah, P., Brouillette, R. et al. Predictors of mortality and length of stay for neonates admitted to children's hospital neonatal intensive care units. J Perinatol 28, 297–302 (2008). https://doi.org/10.1038/sj.jp.7211904
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211904
Keywords
This article is cited by
-
A case-based reasoning system for neonatal survival and LOS prediction in neonatal intensive care units: a development and validation study
Scientific Reports (2023)
-
Benchmarking utilization, length of stay, and complications following minimally invasive repair of major congenital anomalies
Surgical Endoscopy (2022)
-
Metabolic Acidosis in Preterm Infants is Associated with a Longer Length of Stay in the Neonatal Intensive Care Unit
PharmacoEconomics - Open (2020)
-
Rapid whole-genome sequencing decreases infant morbidity and cost of hospitalization
npj Genomic Medicine (2018)
-
Adverse Drug Reactions in Hospitalized Pediatric Patients: A Prospective Observational Study
The Indian Journal of Pediatrics (2016)