Abstract
Background:
We assessed the association of human papillomavirus (HPV) infection and cervical intraepithelial neoplasia (CIN) with various characteristics, CD4 count and use of combination antiretroviral therapy (cART) among HIV-positive women.
Methods:
Cross-sectional study of 498 HIV-positive women who underwent HPV PCR-based testing, cytology, and systematic cervical biopsy.
Results:
In all, 68.7% of women were HPV-positive, 52.6% had high-risk (hr) HPV, and 40.2% multiple type infections. High-risk human papillomavirus-positivity did not vary significantly by age but it was negatively associated with education level. The most frequent types in 113 CIN2/3 were HPV16 (26.5%), HPV35 (19.5%), and HPV58 (12.4%). CD4 count was negatively associated with prevalence of hrHPV (P<0.001) and CIN2/3 among non-users of cART (P=0.013). Combination antiretroviral therapies users (⩾2 year) had lower hrHPV prevalence (prevalence ratio (PR) vs non-users=0.77, 95% confidence interval (CI): 0.61–0.96) and multiple infections (PR=0.68, 95% CI: 0.53–0.88), but not fewer CIN2/3. The positive predictive value of hrHPV-positivity for CIN2/3 increased from 28.9% at age <35 years to 53.3% in ⩾45 years.
Conclusion:
The burden of hrHPV and CIN2/3 was high and it was related to immunosuppression level. Combination antiretroviral therapies ( ⩾2 year) use had a favourable effect on hrHPV prevalence but cART in our population may have been started too late to prevent CIN2/3.
Similar content being viewed by others
Main
Women living with HIV are at increased risk for human papillomavirus (HPV) infection and HPV-related tumours, including cervical intraepithelial neoplasia grade 2 or 3 (CIN2/3) and invasive cervical carcinoma (ICC) (Clifford et al, 2006; De Vuyst et al, 2008). The prevalence of HPV and CIN has been reported to increase with the increase of immunosuppression (Denny et al, 2008; Firnhaber et al, 2010). Combination antiretroviral therapies (cART) against HIV have greatly reduced the incidence of opportunistic infections, Kaposi’s sarcoma, and non-Hodgkin’s lymphoma, but not the incidence of HPV-associated cervical and anal carcinomas (Franceschi et al, 2010). This is perhaps not surprising as HPV-associated carcinomas have a long latent phase. A favourable effect of cART on HPV infection and cervical pre-cancerous lesions has been shown in some (Paramsothy et al, 2009; Minkoff et al, 2010), but not all studies (Bratcher and Sahasrabuddhe, 2010; Shrestha et al, 2010) on the topic.
A favourable effect of cART on cervical cancer and its precursor lesions would be of particular importance in sub-Saharan Africa (SSA), home to three quarters of women living with HIV (WHO, 2011), and 14% of cervical cancer cases worldwide (Ferlay et al, 2010). Access to cART has recently been greatly improved in SSA and by the end of 2010 nearly half of the people who need cART in SSA have had access to it (WHO, 2011). Access to cervical screening is also improving among HIV-positive women in SSA (Brower, 2011), but to a much lesser extent than that to cART.
Human papillomavirus testing has been shown to be superior to cytological screening in terms of sensitivity and duration of negative predictive value against CIN2/3 and cervical cancer in the general female population in high- and low-resource countries (Sankaranarayanan et al, 2009; Ronco et al, 2010; Rijkaart et al, 2012). The use of HPV testing in HIV-positive women and, by and large, in very high HPV prevalence populations have created, however, concerns due to the low test specificity in these settings (Giorgi-Rossi et al, 2012), and hence, the heavy burden of the management of HPV-positive women (Kitchener et al, 2007). Scanty data are available on the detection of high-grade lesions through HPV testing in under-screened populations (Keita et al, 2009; Gage et al, 2012), including in HIV-positive women (Denny et al, 2008; Singh et al, 2009).
The aims of this cross-sectional study from Nairobi, Kenya, were to assess: (1) the distribution of different HPV types at baseline in a cohort of HIV-positive women; (2) the association of high-risk (hr) HPV infection and CIN2/3 with various host factors, including age, CD4 count, and cART use; and (3) the positive predictive value (PPV) of HPV testing in HIV-positive women.
Materials and methods
Participants and study procedures
In 2009, 498 HIV-positive women in Nairobi, Kenya were included as part of a study comparing cervical cancer screening methods. Women who attended the Coptic Hope Center for Infectious Diseases for HIV-related conditions were invited to participate in the study and were eligible if they were: between 18 and 55 years of age; not screened in the last year; and never treated for cervical cancer or pre-cancerous lesions. Women received cervical cancer screening with conventional cytology, visual inspection with acetic acid, and HPV testing (Chung et al, 2011a, 2011b). The characteristics of these women at baseline are the object of the present report.
After obtaining a written informed consent, information on clinical and lifestyle characteristics of study women was collected. A venous blood sample was taken to measure CD4 count. Cervical exfoliated cells were collected by a nurse using a Cervex-Brush (Rovers Medical Devices, Oss, The Netherlands) and placed in PreservCyt medium (Hologic, Marlborough, MA, USA) for HPV testing. A medical doctor performed a colposcopic examination and took a biopsy from all women, either from the most abnormal area on the cervix identified by the colposcopic examination, or at 12 o’clock if no lesion was visualised, as this position is the most frequent location for cervical lesions. Biopsy tissues were immediately immersed in 10%-buffered formalin and transported to the pathology laboratory, where they were embedded in paraffin. Cervical disease status in this study was based on biopsy results. Twenty-seven women with inadequate biopsy results had, therefore, to be excluded in the analyses that included histological findings (Tables 1, 4 and 5).
As per Kenyan national guidelines, free cART should have started if: (1) CD4 count was <250 cells μl−1; (2) World Health Organisation (WHO) clinical stage was IV; (3) CD4 count was <350 cells μl−1 and WHO clinical stage was III (Ojoo, 2007). However, full information on history of cART use, CD4 count at beginning of cART, and adherence to treatment was not available in the present study.
The study protocol was approved by the Ethical Review Committees of the Kenyatta National Hospital, Kenya, the University of Washington, USA, and the International Agency for Research on Cancer, France.
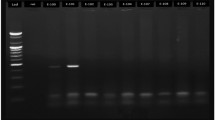
Human papillomavirus DNA testing
Human papillomavirus samples were stored at ambient temperature and shipped to the Department of Pathology of the Vrije University Medical Centre, Amsterdam, The Netherlands for HPV DNA testing. Testing was done on exfoliated cells, according to a protocol similar to that used in previous IARC HPV prevalence surveys (Clifford et al, 2005). Beta-globin polymerase chain reaction (PCR) analysis was performed in order to assess the DNA quality. The presence of HPV DNA was first determined using general primer GP5+/6+-mediated PCR (Jacobs et al, 2000). Polymerase chain reaction products were hybridised using an enzyme immunoassay (EIA) that included two oligoprobes: one for hrHPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68 and another for low-risk HPV types 6, 11, 26, 30, 32, 34, 40, 42, 43, 44, 53, 54, 55, 57, 61, 64, 67, 69, 70, 71, 72, 73, 81, 82/mm4, 82/is39, 83, 84, 85, 86, 89, and 90. Subsequent HPV typing was performed by reverse-line blot hybridisation of PCR products, as described previously (van den Brule et al, 2002). Human papillomavirus types of IARC classification group 1 ‘carcinogenic to humans’ (HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59) and group 2A ‘probably carcinogenic to humans’ (HPV68) were considered as hr types (Schiffman et al, 2009). All other HPV types were considered low-risk types. Samples that were positive at hr EIA, but did not reveal positivity in the typing assay were classified as uncharacterised hrHPV types. One sample was negative for beta-globin, but positive for HPV DNA, and hence remained included in the analysis.
Cytology and histology
Cytological slides and biopsies were processed by staff under the supervision of the study pathologist (FR) at the Aga Khan University of Nairobi, who also read all of the cytological and histological slides. Cytology was reported according to the Bethesda 1991 revised classification (Luff, 1992).
Statistical analysis
Prevalence ratios (PRs) and corresponding 95% confidence intervals (CIs) of HPV infection by different characteristics were computed using a binomial regression model with a log link (as opposed to the logistic link used to compute odds ratios) adjusted for age group (<30; 30–34; 35–39; 40–44; ⩾45). Prevalence ratios for HPV infection (any hr types and multiple types) and CIN2/3 were computed by cART use and by CD4 count (overall and stratified by cART use). Prevalence ratios for CIN1 and CIN2/3 among hrHPV-positive women by the age groups were computed with adjustment for CD4 (<250; 250–499; ⩾500 cells μl−1), cART use (never, <2 years, ⩾2 years), and previous screening. Tests for linear trend of PRs were computed giving an increasing score for each level of the categorised variable and fitting them into the model as continuous variables.
Results
The mean age of 498 study women was 38.1 years (5–95% percentiles: 27–51). Among women with adequate biopsy results, 172 (36.5%) had a normal histology. Cervical intraepithelial neoplasia 1 was detected in 186 women (39.5%); CIN2 in 66 (14.0%); and CIN3 in 47 (10.0%). No ICCs were found.
Table 1 shows the prevalence of HPV types by histological findings and overall. In total, 68.7% of women were HPV-positive, 52.6% were infected with hrHPV types, and 40.2% had multiple infections. High-risk human papillomavirus types were found in 88.0% of multiple infections. Human papillomavirus prevalence was 90.3% in women with CIN2/3. The most frequently found HPV types among women with normal histology were HPV35 (9.9%), HPV52 (7.6%), HPV56 (6.4%), HPV18, and HPV31 (both 5.2%). The prevalence of individual HPV types in women with CIN1 was similar as among women with normal histology, except for an excess of HPV16. HPV16 (26.5%), HPV35 (19.5%), HPV58 (12.4%), and HPV18 and HPV31 (both 10.6%) were the most frequently detected types in women with CIN2/3.
Prevalence ratios for hrHPV-positivity by selected characteristics are shown in Table 2. High-risk human papillomavirus prevalence decreased only slightly with age from 61.3% in women <30 years to 49.5% in women ⩾45 years (Ptrend PR=0.136). Women with higher education had a significantly lower HPV prevalence, compared with women with primary education only or no education (PR=0.74; 95% CI: 0.58–0.95). Positivity for hrHPV was not associated with marital status, number of lifetime or recent partners, use of hormonal contraceptives or number of pregnancies. All findings in Table 2 were similar when positivity for any HPV instead of hrHPV types was assessed.
Figure 1 shows age-specific prevalence of HPV (classified hierarchically into HPV16 and/or 18, hrHPV types but not HPV 16/18, and low-risk types only), and of multiple HPV infections. No significant trends in positivity for HPV 16/18, other hr, low-risk types, and multiple infections were found by age group.
CD4 count at recruitment was 407, 333, and 483 cells μl−1, in women who had never used cART or had used cART for <2 years, or ⩾2 years, respectively (data not shown). The presence of hrHPV infection according to CD4 count (overall and stratified by cART use) and cART use is shown in Table 3. High-risk human papillomavirus-positivity was higher in women with CD4 counts <250 cells μl−1 (PR vs CD4 counts ⩾500 cells μl−1=1.46; 95% CI: 1.18–1.82). The association of CD4 count with hrHPV-positivity was similar in cART users and non-users, although linear trend was significant among cART non-users only. Compared with non-users, cART users for 2 years or longer were less likely to be hrHPV-positive (PR=0.77, 95% CI: 0.61–0.96). Multiple HPV infections were also more frequent in women with CD4 count <250 cells μl−1 (PR vs CD4 count ⩾500 cells μl−1=1.89; 95% CI: 1.43–2.50), and less frequent in women with ⩾2-year cART use (PR vs non-users=0.68, 95% CI: 0.53–0.88) (data not shown).
Detection of CIN2/3, according to CD4 count (overall and stratified by cART use) and cART use is shown in Table 4. Cervical intraepithelial neoplasia 2/3 presence increased significantly from 17.2% in women with CD4 count ⩾500 cells μl−1 to 30.7% in women with CD4 count <250 cells μl−1 (PR=1.66; 95% CI: 1.05–2.64). Stratification by cART use showed, however, that the inverse association between CD4 count and CIN2/3 prevalence was restricted to non-cART users (PR=4.23; 95% CI: 1.27–14.07). Use of cART was not associated with CIN2/3 detection.
Table 5 shows the age-specific detection of CIN1 and CIN2/3 among hrHPV-positive women, which is equivalent to the clinical PPV of hrHPV testing for the corresponding diagnoses. The detection of CIN1 decreased from 40.0% in women <35 years to 22.2% in women ⩾45 years (Ptrend PR=0.122). Conversely, the proportion of CIN2/3 in hrHPV-positives increased significantly from 28.9% below age 35 to 53.3% at age 45 or older (PR=1.71; 95% CI: 1.10–2.66). CIN2/3-to-CIN1 ratio increased, among hrHPV-positive women, therefore, from 0.7 below age 35 to 2.4 at age 45 years or older.
Discussion
Human immunodeficiency virus-positive women in our present study had a very high prevalence of HPV infections (68.7%), notably hrHPV type (52.6%), and multiple infections (40.2%). The availability of cervical biopsy in all study participants led to the detection of CIN2/3 in 37.5% of hrHPV-positive women. Cervical intraepithelial neoplasia 2/3 detection and, hence, the PPV of hrHPV-positivity, increased with age. High CD4 count and prolonged cART use were significantly associated with lower prevalence of hrHPV infection. CD4 count was inversely related to CIN2/3 detection only among women who had never used cART and cART use had no clear impact on CIN2/3 presence.
Elevated prevalence of HPV (50% or more) and high-grade lesions were consistently reported in HIV-positive women in SSA (Clifford et al, 2006; Singh et al, 2009; Firnhaber et al, 2010; Djigma et al, 2011; Tobian et al, 2011), as well as in high-resource countries (Clifford et al, 2006; Paramsothy et al, 2009). We compared the prevalence of selected HPV types in HIV-positive women in our study with that in women from the general population in Africa, using a large meta-analysis (Guan et al, 2012). The more than two-fold higher HPV prevalence among histologically normal women in our study than in Guan et al was mainly accounted for by hr types other than HPV16. Our findings are consistent with a report from the two US cohorts in which the prevalence and incidence of HPV16 in HIV-positive women was more weakly associated with a woman’s immune status than that of other hrHPV types (Strickler et al, 2003). Human papillomavirus 16 was the most frequently detected type (29.4%) in HPV-positive CIN2/3 lesions in our present study in agreement with the findings of the meta-analysis for high-grade lesions in Africa (30.3%) (Guan et al, 2012). The proportion of HPV18 in HPV-positive women with different histological findings was well comparable in our study and the meta-analysis (e.g., 10.6% and 9.2%, respectively in women with high-grade cervical lesions) (Guan et al, 2012). Human papillomavirus 16 was found in 23% of high-grade intraepithelial lesions among HIV-positive women in Rwanda (Singh et al, 2009), and 42% in South Africa (Firnhaber et al, 2010).
In our present study, the prevalence of any HPV type, hr types, and the proportion of multiple HPV infections was similar across all the age groups in agreement with a few studies of the general female populations in SSA (Keita et al, 2009; De Vuyst et al, 2010; Clarke et al, 2011) and among HIV-positive women in SSA and high-resource countries.
We found no significant risk factors for hrHPV-positivity except for a moderate negative association with educational level. Although self-reported sexual behaviour has serious limitations, a lack of association of hrHPV-positivity with the number of lifetime or recent sexual partners may be explained by a stronger role of impaired clearance and reactivation than increased HPV acquisition in HIV-positive women (Strickler et al, 2003). It is also possible that influence of sexual behaviour is obscured by the extremely high hrHPV prevalence in HIV-positive women. Twenty-three percent of women did not provide information on lifetime number of sexual partners. They did not have, however, an increased risk for hrHPV infection (PR=0.78; 95% CI: 0.61–1.01).
Low CD4 count was associated with higher positivity for hrHPV and multiple HPV infections, consistently among cART users and non-users, in agreement with a few previous reports (Strickler et al, 2005; Denny et al, 2008; Singh et al, 2009; Firnhaber et al, 2010). To date, only few studies have been able to show an impact of cART on HPV infection (Paramsothy et al, 2009; Bratcher and Sahasrabuddhe, 2010; Minkoff et al, 2010). Two years cART treatment or longer was also associated with lower prevalence of hr and multiple HPV infections in our study. The need for relatively long-duration cART use to diminish HPV burden may derive from the fact that immune reconstitution after initiation of cART occurs through different phases. It starts mainly with an immediate re-distribution of memory T-cells from the lymphoid tissues and it is followed by an expansion of naive T-cells from the thymus that may be active against new pathogens. The latter process takes months to years after cART initiation (Corbeau and Reynes, 2011).
CD4 count was inversely associated with CIN2/3 presence only in women who had never been on cART. In fact, cART use rapidly modifies CD4 count and makes current CD4 uninformative in respect to the past burden of immunosuppression. Lack of clear beneficial impact of cART on CIN2/3 detection in our study may suggest that immune reconstitution by cART was not able to prevent or reverse the development of CIN2/3 possibly because it was not established sufficiently early in time after HPV infection. Unfortunately, our study did not include information on CD4 count at the start of cART and adherence with treatment.
Concerns were expressed on the lack of specificity of HPV testing in HIV-positive women, due to very high hrHPV prevalence. We explored, therefore, for the first time in HIV-positive women, the PPV of hrHPV-positive results for CIN2/3 in the different age groups. The PPV for CIN2/3 was high across all the age groups but it reached 53% in women aged 45 years or older as CIN2/3 accumulate over time in inadequately screened women (Gage et al, 2012). High PPV demonstrates the effectiveness and potential cost-effectiveness (Vanni et al, 2012) of HPV testing HIV-positive women despite low test specificity (Kuhn et al, 2010; Giorgi-Rossi et al, 2012). A modelling study showed that, at a cost of 13 USD per test, yearly screening using the HPV hybrid-capture2 test followed by cytology was very cost-effective, in respect to the current yearly cytology screening in HIV-positive women in Brazil (Vanni et al, 2012). The advent of a low-cost rapid HPV test in the near future will favour the cost-effectiveness of HPV testing even more.
The greatest strength of our present study is the availability of a biopsy for all women, regardless of cytological findings. An additional strength is the use of a well-validated and widely used HPV test (Clifford et al, 2006; Guan et al, 2012) whose findings were ignored by the local pathologist. Weaknesses include the cross-sectional nature of our present findings that did not allow to investigate the effects of CD4 count and cART on HPV infection and CIN2/3 longitudinally. Unfortunately we were also not able to collect information on either CD4 at the beginning of cART or adherence to treatment, that is, information that would have especially helped interpreting our findings on cART and CIN2/3 prevalence. Finally, although we had a sufficiently large number of HIV-positive women to describe HPV type distribution overall and by CIN presence, some potentially informative subgroups were small (e.g., women with CD4 ⩾500 cells μl−1).
In conclusion, the burden of hrHPV and CIN2/3 in HIV-positive women in Kenya was high and it was related to immunosuppression level. Combination antiretroviral therapies (⩾2 year) use had a favourable effect on hrHPV prevalence but antiretroviral treatment in our study population may have been started too late to prevent or reverse CIN2/3. Timely initiation of cART may ultimately decrease cervical cancer in HIV-positive women. Access to HPV vaccination and cervical screening using HPV testing in SSA are needed to reduce cervical cancer among HIV-positive women.
Change history
11 October 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bratcher LF, Sahasrabuddhe VV (2010) The impact of antiretroviral therapy on HPV and cervical intraepithelial neoplasia: current evidence and directions for future research. Infect Agent Cancer 5: 8
Brower V (2011) AIDS-related cancers increase in Africa. J Natl Cancer Inst 103: 918–919
Chung MH, McKenzie KP, De Vuyst H, Pamnani R, Rana F, Njoroge JW, John-Steward G, Richardson B, Sakr S, Mugo NR (2011a) Comparing visual inspection with acetic acid, high-risk HPV testing, and Pap smear to colposcopic biopsy among HIV+ women. 18th Conference on Retroviruses and Opportunistic Infections; Boston, USA; 27 February–2 March 2011. Presentation 41 [Abstract]
Chung MH, McKenzie KP, Richardson BA, John-Stewart GC, Coombs RW, De Vuyst H, Njoroge JW, Nyongesa-Malava E, Sakr SR, Mugo NR (2011b) Cervical HIV-1 RNA shedding after cryotherapy among HIV-positive women with cervical intraepithelial neoplasia stage 2 or 3. AIDS 25: 1915–1919
Clarke MA, Gage JC, Ajenifuja KO, Wentzensen NA, Adepiti AC, Wacholder S, Burk RD, Schiffman M (2011) A population-based cross-sectional study of age-specific risk factors for high risk human papillomavirus prevalence in rural Nigeria. Infect Agent Cancer 6: 12
Clifford GM, Gallus S, Herrero R, Muñoz N, Snijders PJ, Vaccarella S, Anh PT, Ferreccio C, Hieu NT, Matos E, Molano M, Rajkumar R, Ronco G, de Sanjosé S, Shin HR, Sukvirach S, Thomas JO, Tunsakul S, Meijer CJ, Franceschi S (2005) Worldwide distribution of human papillomavirus types in cytologically normal women in the International Agency for Research on Cancer HPV prevalence surveys: a pooled analysis. Lancet 366: 991–998
Clifford GM, Goncalves MA, Franceschi S (2006) Human papillomavirus types among women infected with HIV: a meta-analysis. AIDS 20: 2337–2344
Corbeau P, Reynes J (2011) Immune reconstitution under antiretroviral therapy: the new challenge in HIV-1 infection. Blood 117: 5582–5590
De Vuyst H, Lillo F, Broutet N, Smith JS (2008) HIV, human papillomavirus, and cervical neoplasia and cancer in the era of highly active antiretroviral therapy. Eur J Cancer Prev 17: 545–554
De Vuyst H, Parisi MR, Karani A, Mandaliya K, Muchiri L, Vaccarella S, Temmerman M, Franceschi S, Lillo F (2010) The prevalence of human papillomavirus infection in Mombasa, Kenya. Cancer Causes Control 21: 2309–2313
Denny L, Boa R, Williamson AL, Allan B, Hardie D, Stan R, Myer L (2008) Human papillomavirus infection and cervical disease in human immunodeficiency virus-1-infected women. Obstet Gynecol 111: 1380–1387
Djigma FW, Ouedraogo C, Karou DS, Sagna T, Bisseye C, Zeba M, Ouermi D, Gnoula C, Pietra V, Ghilat-Avoid-Belem NW, Sanogo K, Sempore J, Pignatelli S, Ferri AM, Nikiema JB, Simpore J (2011) Prevalence and genotype characterization of human papillomaviruses among HIV-seropositive in Ouagadougou, Burkina Faso. Acta Trop 117: 202–206
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) GLOBOCAN 2008. Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10. International Agency for Research on Cancer: Lyon, France, Available from http://globocan.iarc.fr
Firnhaber C, Van Le H, Pettifor A, Schulze D, Michelow P, Sanne IM, Lewis DA, Williamson AL, Allan B, Williams S, Rinas A, Levin S, Smith JS (2010) Association between cervical dysplasia and human papillomavirus in HIV seropositive women from Johannesburg South Africa. Cancer Causes Control 21: 433–443
Franceschi S, Lise M, Clifford GM, Rickenbach M, Levi F, Maspoli M, Bouchardy C, Dehler S, Jundt G, Ess S, Bordoni A, Konzelmann I, Frick H, Dal Maso L, Elzi L, Furrer H, Calmy A, Cavassini M, Ledergerber B, Keiser O (2010) Changing patterns of cancer incidence in the early- and late-HAART periods: the Swiss HIV Cohort Study. Br J Cancer 103: 416–422
Gage JC, Ajenifuja KO, Wentzensen NA, Adepiti AC, Eklund C, Reilly M, Hutchinson M, Wacholder S, Harford J, Soliman AS, Burk RD, Schiffman M (2012) The age-specific prevalence of human papillomavirus and risk of cytologic abnormalities in rural Nigeria: implications for screen-and-treat strategies. Int J Cancer 130: 2111–2117
Giorgi-Rossi P, Franceschi S, Ronco G (2012) HPV prevalence and accuracy of HPV testing to detect high-grade cervical intraepithelial neoplasia. Int J Cancer 130: 1387–1394
Guan P, Howell-Jones R, Li N, Bruni L, de Sanjosé S, Franceschi S, Clifford GM (2012) Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer (in press)
Jacobs MV, Walboomers JM, Snijders PJ, Voorhorst FJ, Verheijen RH, Fransen-Daalmeijer N, Meijer CJ (2000) Distribution of 37 mucosotropic HPV types in women with cytologically normal cervical smears: the age-related patterns for high-risk and low-risk types. Int J Cancer 87: 221–227
Keita N, Clifford GM, Koulibaly M, Douno K, Kabba I, Haba M, Sylla BS, van Kemenade FJ, Snijders PJ, Meijer CJ, Franceschi S (2009) HPV infection in women with and without cervical cancer in Conakry, Guinea. Br J Cancer 101: 202–208
Kitchener H, Nelson L, Adams J, Mesher D, Sasieni P, Cubie H, Moore C, Heard I, Agarossi A, Casolati E, Denny L, Bradbeer C, Lyons F, Beattie G, Niemiec T (2007) Colposcopy is not necessary to assess the risk to the cervix in HIV-positive women: an international cohort study of cervical pathology in HIV-1 positive women. Int J Cancer 121: 2484–2491
Kuhn L, Wang C, Tsai WY, Wright TC, Denny L (2010) Efficacy of human papillomavirus-based screen-and-treat for cervical cancer prevention among HIV-infected women. AIDS 24: 2553–2561
Luff RD (1992) The Bethesda System for reporting cervical/vaginal cytologic diagnoses. Report of the 1991 Bethesda workshop. Am J Clin Pathol 98: 152–154
Minkoff H, Zhong Y, Burk RD, Palefsky JM, Xue X, Watts DH, Levine AM, Wright RL, Colie C, D'Souza G, Massad LS, Strickler HD (2010) Influence of adherent and effective antiretroviral therapy use on human papillomavirus infection and squamous intraepithelial lesions in human immunodeficiency virus-positive women. J Infect Dis 201: 681–690
Ojoo S (2007) Kenya National Clinical Manual for ART Providers: A Concise and Practical Guide to ART Provision 2nd edition. National AIDS and STI Control Program (NASCOP): Nairobi, 70 p
Paramsothy P, Jamieson DJ, Heilig CM, Schuman PC, Klein RS, Shah KV, Rompalo AM, Cu-Uvin S, Duerr A (2009) The effect of highly active antiretroviral therapy on human papillomavirus clearance and cervical cytology. Obstet Gynecol 113: 26–31
Rijkaart DC, Berkhof J, Rozendaal L, van Kemenade FJ, Bulkmans NW, Heideman DA, Kenter GG, Cuzick J, Snijders PJ, Meijer CJ (2012) Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol 13: 78–88
Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Palma PD, Del Mistro A, Ghiringhello B, Girlando S, Gillio-Tos A, De Marco L, Naldoni C, Pierotti P, Rizzolo R, Schincaglia P, Zorzi M, Zappa M, Segnan N, Cuzick J (2010) Efficacy of human papillomavirus testing for the detection of invasive cervical cancers and cervical intraepithelial neoplasia: a randomised controlled trial. Lancet Oncol 11: 249–257
Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, Hingmire S, Malvi SG, Thorat R, Kothari A, Chinoy R, Kelkar R, Kane S, Desai S, Keskar VR, Rajeshwarkar R, Panse N, Dinshaw KA (2009) HPV screening for cervical cancer in rural India. N Engl J Med 360: 1385–1394
Schiffman M, Clifford G, Buonaguro FM (2009) Classification of weakly carcinogenic human papillomavirus types: addressing the limits of epidemiology at the borderline. Infect Agent Cancer 4: 8
Shrestha S, Sudenga SL, Smith JS, Bachmann LH, Wilson CM, Kempf MC (2010) The impact of highly active antiretroviral therapy on prevalence and incidence of cervical human papillomavirus infections in HIV-positive adolescents. BMC Infect Dis 10: 295
Singh DK, Anastos K, Hoover DR, Burk RD, Shi Q, Ngendahayo L, Mutimura E, Cajigas A, Bigirimani V, Cai X, Rwamwejo J, Vuolo M, Cohen M, Castle PE (2009) Human papillomavirus infection and cervical cytology in HIV-infected and HIV-uninfected Rwandan women. J Infect Dis 199: 1851–1861
Strickler HD, Burk RD, Fazzari M, Anastos K, Minkoff H, Massad LS, Hall C, Bacon M, Levine AM, Watts DH, Silverberg MJ, Xue X, Schlecht NF, Melnick S, Palefsky JM (2005) Natural history and possible reactivation of human papillomavirus in human immunodeficiency virus-positive women. J Natl Cancer Inst 97: 577–586
Strickler HD, Palefsky JM, Shah KV, Anastos K, Klein RS, Minkoff H, Duerr A, Massad LS, Celentano DD, Hall C, Fazzari M, Cu-Uvin S, Bacon M, Schuman P, Levine AM, Durante AJ, Gange S, Melnick S, Burk RD (2003) Human papillomavirus type 16 and immune status in human immunodeficiency virus-seropositive women. J Natl Cancer Inst 95: 1062–1071
Tobian AA, Kong X, Wawer MJ, Kigozi G, Gravitt PE, Serwadda D, Eaton KP, Nalugoda F, Quinn TC, Gray RH (2011) Circumcision of HIV-infected men and transmission of human papillomavirus to female partners: analyses of data from a randomised trial in Rakai, Uganda. Lancet Infect Dis 11: 604–612
van den Brule AJ, Pol R, Fransen-Daalmeijer N, Schouls LM, Meijer CJ, Snijders PJ (2002) GP5+/6+ PCR followed by reverse line blot analysis enables rapid and high-throughput identification of human papillomavirus genotypes. J Clin Microbiol 40: 779–787
Vanni T, Luz PM, Grinsztejn B, Veloso VG, Foss A, Mesa-Frias M, Legood R (2012) Cervical cancer screening among HIV-infected women: an economic evaluation in a middle-income country. Int J Cancer 131: E96–104
WHO (2011) Global HIV/AIDS response: Progress report 2011. Key facts on HIV epidemic and progress in regions and countries in 2010, sub-Saharan Africa. Available at http://www.who.int/hiv/pub/progress_report2011/regional_facts/en/index.html. Accessed August 2012
Acknowledgements
We thank the research personnel, clinic and laboratory staff, and data management teams in Nairobi, Kenya; Seattle, USA; Amsterdam, The Netherlands; and Lyon, France for their work. We recognise the Coptic Hope Centre for Infectious Diseases, for their cooperation and our patients for their participation and support. This work was funded by the Washington Global Health Alliance, the National Institutes of Health (grant number 5K23AI065222-04), a grant from the Bill & Melinda Gates Foundation (grant number 35537), and from the Fondation de France (grant number 00016673).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
De Vuyst, H., Mugo, N., Chung, M. et al. Prevalence and determinants of human papillomavirus infection and cervical lesions in HIV-positive women in Kenya. Br J Cancer 107, 1624–1630 (2012). https://doi.org/10.1038/bjc.2012.441
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.441
Keywords
This article is cited by
-
Women diagnosed with HIV and unknown HIV status perceived susceptibility to cervical cancer and perceived benefits of cervical cancer screening in Ghana: a cross-sectional study
BMC Women's Health (2021)
-
A cross-sectional analysis of factors associated with detection of oncogenic human papillomavirus in human immunodeficiency virus-infected and uninfected Kenyan women
BMC Infectious Diseases (2019)
-
Epidemiology of cervical human papillomavirus (HPV) infection and squamous intraepithelial lesions (SIL) among a cohort of HIV-infected and uninfected Ghanaian women
BMC Cancer (2017)
-
Cervical cancer patients presentation and survival in the only oncology referral hospital, Ethiopia: a retrospective cohort study
Infectious Agents and Cancer (2017)
-
Variability of high risk HPV genotypes among HIV infected women in Mwanza, Tanzania- the need for evaluation of current vaccine effectiveness in developing countries
Infectious Agents and Cancer (2016)