Abstract
BACKGROUND
Exacerbations in chronic respiratory diseases (CRDs) are sensitive to seasonal variations in exposure to respiratory infectious agents and allergens and patient factors such as non-adherence. Hence, regular general practitioner (GP) contact is likely to be important in order to recognise symptom escalation early and adjust treatment.
OBJECTIVE
To examine the association of regularity of GP visits with all-cause mortality and first CRD hospitalisation overall and within groups of pharmacotherapy level in older CRD patients.
DESIGN
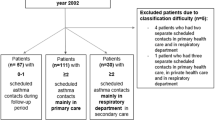
A retrospective cohort design using linked hospital, mortality, Medicare and pharmaceutical data for participant, exposure and outcome ascertainment. GP visit pattern was measured during the first 3 years of the observation period. Patients were then followed for a maximum of 11.5 years for ascertainment of hospitalisations and deaths.
PARTICIPANTS
We studied 108,455 patients aged ≥65 years with CRD in Western Australia (WA) during 1992–2006.
MAIN MEASURES
A GP visit regularity score (range 0–1) was calculated and divided into quintiles. A clinician consensus panel classified levels of pharmacotherapy. Cox proportional hazards models, controlling for multiple factors including GP visit frequency, were used to calculate hazard ratios and confidence intervals.
KEY RESULTS
Differences in survival curves and hospital avoidance pattern between the GP visit regularity quintiles were statistically significant (p = 0.0279 and p < 0.0001, respectively). The protective association between GP visit regularity and death appeared to be confined to the highest pharmacotherapy level group (P for interaction = 0.0001). Higher GP visit regularity protected against first CRD hospitalisation compared with the least regular quintile regardless of pharmacotherapy level (medium regular: HR = 0.84, 95% CI = 0.77–0.92; 2nd most regular: HR = 0.74, 95% CI = 0.67–0.82; most regular HR = 0.77, 95% CI = 0.68–0.86).
CONCLUSIONS
The findings indicate that regular and proactive ‘maintenance’ primary care, as distinct from ‘reactive’ care, is beneficial to older CRD patients by reducing their risks of hospitalisation and death.


Similar content being viewed by others
References
Asthma in Australia 2008. Canberra: Australian centre for asthma monitoring and Australian Institute of Health and Welfare; 2008. Report No.: AIHW cat. no. ACM 14.
Asthma Management Handbook 2006. Melbourne: National Asthma Council Australia; 2006.
Begg S, Vos T, Barker B, Stevenson C, Stanley L, Lopez A. The burden of disease and injury in Australia 2003. Australian Institute of Health and Ageing. Canberra; 2007. Report No.: AIHW cat. no. PHE 82.
Frith PA, Cafarella PA, Duffy JM. Chronic obstructive pulmonary disease (COPD) is a major personal and public health burden in Australia. Aust N Z J Public Health. 2008;32:139–41.
Glasgow N. Systems for the management of respiratory disease in primary care—an international series: Australia. Prim Care Respir J. 2008;17:19–25.
Tsai CL, Griswold SK, Clark S, Camargo CA Jr. Factors associated with frequency of emergency department visits for chronic obstructive pulmonary disease exacerbation. J Gen Intern Med. 2007;22:799–804.
Cree M, Bell NR, Johnson D, Carriere KC. Increased continuity of care associated with decreased hospital care and emergency department visits for patients with asthma. Dis Manag. 2006;9:63–71.
Shi L, Samuels ME, Pease M, Bailey WP, Corley EH. Patient characteristics associated with hospitalizations for ambulatory care sensitive conditions in South Carolina. South Med J. 1999;92:989–98.
Rizza P, Bianco A, Pavia M, Angelillo IF. Preventable hospitalization and access to primary health care in an area of Southern Italy. BMC Health Serv Res. 2007;7:134.
Parchman ML, Culler SD. Preventable hospitalizations in primary care shortage areas. An analysis of vulnerable Medicare beneficiaries. Arch Fam Med. 1999;8:487–91.
Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–11.
Basu J, Friedman B, Burstin H. Primary care, HMO enrollment, and hospitalization for ambulatory care sensitive conditions: a new approach. Med Care. 2002;40:1260–9.
Sunyer J, Anto JM, McFarlane D, et al. Sex differences in mortality of people who visited emergency rooms for asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158:851–6.
Huiart L, Ernst P, Suissa S. Cardiovascular morbidity and mortality in COPD. Chest. 2005;128:2640–6.
Dantzer C, Tessier JF, Nejjari C, Barberger-Gateau P, Dartigues JF. Mortality of elderly subjects with self-reported asthma in a French cohort, 1991–1996. Eur J Epidemiol. 2001;17:57–63.
Bellia V, Pedone C, Catalano F, et al. Asthma in the elderly: mortality rate and associated risk factors for mortality. Chest. 2007;132:1175–82.
Restrepo RD. Use of inhaled anticholinergic agents in obstructive airway disease. Respir Care. 2007;52:833–51.
Phua GC, Macintyre NR. Inhaled corticosteroids in obstructive airway disease. Respir Care. 2007;52:852–8.
Miller-Larsson A, Selroos O. Advances in asthma and COPD treatment: combination therapy with inhaled corticosteroids and long-acting beta 2-agonists. Curr Pharm Des. 2006;12:3261–79.
Yawn BP. Factors accounting for asthma variability: achieving optimal symptom control for individual patients. Prim Care Respir J. 2008;17:138–47.
Walter MJ, Castro M, Kunselman SJ, et al. Predicting worsening asthma control following the common cold. Eur Respir J. 2008;32:1548–54.
Holman CD, Bass AJ, Rouse IL, Hobbs MS. Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health. 1999;23:453–9.
Harris MG, Harris RD. The Australian health system: continuity and change. J Health Hum Serv Adm. 1998;20:442–67.
Medicare Benefits Schedule Book. Canberra: Department of Health and Ageing, Australian government; 2008.
Liu H, Wong L. Data mining tools for biological sequences. J Bioinform Comput Biol. 2003;1:139–67.
Tamim H, Monfared AA, LeLorier J. Application of lag-time into exposure definitions to control for protopathic bias. Pharmacoepidemiol Drug Saf. 2007;16:250–8.
Strom BL. Pharmacoepidemiology. 4th ed. West Sussex: Wiley; 2005.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Patterns of asthma medication use in Australia. Canberra: Australian Centre for Asthma Monitoring and Australian Institute of health and welfare; 2007. Report No.: AIHW cat. no. ACM 11.
Cranston JM, Crockett AJ, Moss JR, Pegram RW, Stocks NP. Models of chronic disease management in primary care for patients with mild-to-moderate asthma or COPD: a narrative review. Med J Aust. 2008;188:S50–2.
Sin DD, Tu JV. Underuse of inhaled steroid therapy in elderly patients with asthma. Chest. 2001;119:720–5.
Schmier JK, Halpern MT, Jones ML. Effects of inhaled corticosteroids on mortality and hospitalisation in elderly asthma and chronic obstructive pulmonary disease patients: appraising the evidence. Drugs Aging. 2005;22:717–29.
Krigsman K, Moen J, Nilsson JL, Ring L. Refill adherence by the elderly for asthma/chronic obstructive pulmonary disease drugs dispensed over a 10-year period. J Clin Pharm Ther. 2007;32:603–11.
Enright PL, McClelland RL, Newman AB, Gottlieb DJ, Lebowitz MD. Underdiagnosis and undertreatment of asthma in the elderly. Cardiovascular Health Study Research Group. Chest. 1999;116:603–13.
Vollmer WM, Peters D, Crane B, Kelleher C, Buist AS. Impact of regular inhaled corticosteroid use on chronic obstructive pulmonary disease outcomes. COPD. 2007;4:135–42.
Sin DD, Tu JV. Inhaled corticosteroids and the risk of mortality and readmission in elderly patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164:580–4.
Sin DD, Tu JV. Inhaled corticosteroid therapy reduces the risk of rehospitalization and all-cause mortality in elderly asthmatics. Eur Respir J. 2001;17:380–5.
Balkrishnan R, Christensen DB. Inhaled corticosteroid use and associated outcomes in elderly patients with moderate to severe chronic pulmonary disease. Clin Ther. 2000;22:452–69.
Radeos MS, Leak LV, Lugo BP, Hanrahan JP, Clark S, Camargo CA Jr. Risk factors for lack of asthma self-management knowledge among ED patients not on inhaled steroids. Am J Emerg Med. 2001;19:253–9.
Goeman DP, Aroni RA, Sawyer SM, et al. Back for more: a qualitative study of emergency department reattendance for asthma. Med J Aust. 2004;180:113–7.
Fernandes AK, Mallmann F, Steinhorst AM, et al. Characteristics of acute asthma patients attended frequently compared with those attended only occasionally in an emergency department. J Asthma. 2003;40:683–90.
Adams RJ, Smith BJ, Ruffin RE. Factors associated with hospital admissions and repeat emergency department visits for adults with asthma. Thorax. 2000;55:566–73.
Acknowledgements
We thank the Australian Department of Health and Ageing, Medicare Australia, the Australian Electoral Commission, the WA Department of Health and the Registrar Generals Office of WA for providing the data used for this investigation. We are furthermore grateful to the Data Linkage Branch of the WA Department of Health for extracting and linking the data. We also thank the clinical consensus panel for designing guidelines for the pharmacotherapy level classification. The research was supported by a project grant from Australia’s National Health and Medical Research Council.
Conflict of Interest: None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
We thank the Australian Department of Health and Ageing, Medicare Australia, the Australian Electoral Commission, the WA Department of Health and the Registrar Generals Office of WA for providing the data used for this investigation. We are furthermore grateful to the Data Linkage Branch of the WA Department of Health for extracting and linking the data. We also thank the clinical consensus panel for designing guidelines for the pharmacotherapy level classification. The research was supported by a project grant from Australia’s National Health and Medical Research Council.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
ESM Table 1
Unadjusted association between GP visit regularity of patients with CRD and risk of death and first CRD hospitalisation, overall and by pharmacotherapy level. (DOC 36 kb)
Rights and permissions
About this article
Cite this article
Einarsdóttir, K., Preen, D.B., Emery, J.D. et al. Regular Primary Care Lowers Hospitalisation Risk and Mortality in Seniors with Chronic Respiratory Diseases. J GEN INTERN MED 25, 766–773 (2010). https://doi.org/10.1007/s11606-010-1361-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1361-6