Abstract
To assess the effectiveness of an alcohol brief intervention administered to violent offenders in a judicial (Magistrates’ court) setting, a randomised controlled trial was conducted. Participants (n = 269) were men aged 16–35 years, who resided within a 30-mile radius of Cardiff, UK, and who had been sentenced for a violent offence committed whilst intoxicated with alcohol. Recruitment occurred on-site. Participants were randomly allocated to receive an alcohol brief intervention (n = 135) or to a control group (n = 134). Objective measures comprised re-offending and injury rates. Self-reported outcome measures comprised Alcohol Use Disorders Identification Test (AUDIT); number of drinking days in the past 3 months; total weekly standard units of alcohol; and stage of change with respect to alcohol consumption (as measured by the Readiness to Change Questionnaire). Participants were followed up 3 months (n = 234; 87%) and 12 months (n = 202; 75.1%) after sentence. No significant between-group differences were observed in any of the alcohol measures or in re-offending. Injury was significantly less likely in offenders who had received the intervention (27.4%) than those who had not [39.6%; 95% confidence interval (CI) = −0.23, −0.009]. At 3-month follow-up, significantly more participants in the intervention group (31%; n = 37) than control group (16%; n = 18) demonstrated an increase in their readiness to change drinking behaviour (χ2 = 8.56; df = 2; P = 0.014), but this did not persist at 12-month follow-up.
Similar content being viewed by others
Introduction
Alcohol-related violence is currently a major problem, high on the agenda of many governments. The association between excessive alcohol consumption and violence has been well established. In a literature review, Collins and Messerschmidt (1993) drew the following conclusions relating to the association between alcohol and violence: (1) up to 82% of violent offenders had consumed alcohol prior to committing an offence; (2) up to 40% of assault victims had been drinking prior to the assault; (3) men are far more likely than women to be both offenders and victims in alcohol-related assaults; (4) men under the age of 30 years are more likely to be involved in alcohol-related assaults than any other demographic group. Recent studies have also supported strong associations between alcohol and violence (Borges et al. 2004; White and Chen 2002; Fergusson and Horwood 2000), even when confounding factors have been taken into consideration.
Brief interventions have resulted in alcohol reduction among problem drinkers across health care settings and socio-cultural groups [World Health Organisation (WHO) 1996]. A WHO review found that, on average, 21% of those who drank alcohol at risky levels and who received a simple 5-minute intervention decreased their alcohol consumption by a significant degree. Consistent with this, The Effective Health Care Review Team (1993) carried out a meta-analysis of brief alcohol interventions and concluded that they were effective in reducing alcohol consumption by up to 20% in people with risky alcohol consumption levels. A more recent meta-analysis of randomised controlled trials concerned with brief interventions (Wilk et al. 1997) concluded that people who were administered a brief intervention were twice as likely to have reduced their alcohol consumption 1 year after having the intervention as those who did not receive an intervention. Furthermore, it has been demonstrated that brief alcohol interventions are an extremely cost effective way of helping those with alcohol problems (Bien et al. 1993).
Brief interventions have proven to be effective in a range of settings, including Emergency Departments (Wright et al. 1998; Gentilello et al. 1999); schools (Werch et al. 2000); primary care (Monteiro and Gomel 1998); general practice (Dyehouse and Sommers 1998; Wallace et al. 1988) and cultures (Cordoba et al. 1998; Bien et al. 1993; WHO Brief Intervention Study Group 1996). However, the findings in the literature are not consistent. For example, Richmond et al. (2000) found that brief interventions administered to postal service workers in Australia were successful in reducing alcohol consumption 10 months after the intervention among women, but not men. In their review of brief interventions administered in general hospital settings, Emmen and colleagues found that, of eight studies that fulfilled the inclusion criteria (many of which were identified as having methodological weaknesses), reduction in alcohol consumption was demonstrated in the intervention group in only one study (2004).
Despite close links between alcohol and violence and disorder, no research evaluating the effectiveness of brief alcohol interventions in offenders or with the violent alcohol abuser in a criminal justice setting has been carried out. Of key strategic importance in this research is that the targeting of relatively young offenders may help those at an early stage of their offending careers, before alcohol dependence has been established. The aim of this randomised controlled trial was to assess the effectiveness of an alcohol brief intervention administered to young violent offenders in a judicial (Magistrates’ court) setting. Specifically, it was hypothesised that a brief alcohol intervention delivered at a Magistrates’ court would reduce: (1) violent offending; (2) alcohol misuse; (3) assault-related and unintentional injury.
Method
Design
This study was a randomised controlled trial, reported here according to the revised guidelines of the Consolidated Standards for Reporting Trials (CONSORT) (Moher et al. 2001), and was approved by the Local Research Ethics Committee (LREC). The CONSORT guidelines are an evidence-based minimum set of recommendations for reporting randomised controlled trials that facilitate consistency of reporting trial findings (Moher et al. 2001).
Setting
Participants were recruited on-site at Cardiff Magistrates’ Court, immediately following sentencing. Screening and administration of interventions also occurred on-site.
Participants (eligibility criteria)
Men aged 16–35 years who had been convicted of a violent offence that was committed whilst they were intoxicated with alcohol, and who lived in a permanent residence within a 30-mile radius of Cardiff, were approached for participation in this study between September 2002 and September 2003. The sample was restricted geographically because of the requirement for face-to-face follow-up interviews at 3 months and 12 months. Offences that constituted violent offences for the purposes of this study are listed in Table 1.
Participant selection
Each day, a list of the offences scheduled to be heard the following day was obtained by the project manager. From this, a daily register of violent offence charges involving men aged 16–35 years, living within a 30-mile radius of Cardiff, was constructed. The project manager contacted the Crown Prosecution Service (CPS) in order to determine which of these violent offences were alcohol related. For offences where the CPS had no information about alcohol involvement in an offence, the court research team attempted to gain this information from relevant solicitors and/or the CPS at court the following day.
At the end of each day, data about all violent offences scheduled for consideration that day were entered into a study database comprising name, date of birth, nature of offence(s), alcohol involvement, and outcome (e.g. recruitment, refusal, charge dropped; case transferred to Crown Court). This database was referred to throughout data collection to assist in the construction of the daily register of violent offences to check whether a defendant had already been recruited, or whether information about the involvement of alcohol in the offence was already known.
Recruitment
The majority of participants were recruited by the project’s research nurse, but the project manager and two other interviewers assisted. The research team liaised closely with defence solicitors, as offenders were often distrustful and/or resentful of anyone else. Wherever possible, a researcher was introduced to the offender in the presence of the defendant’s solicitor immediately after the defendant had been sentenced and had left the court-room. The purpose and nature of the project were briefly described to the participant. Written consent for inclusion in the study was obtained, as well as for a member of the research team to check the participant’s medical records (for injury data) and the Police National Crime Database (for re-offending data). Participants provided their contact details, together with details of at least one secondary reliable contact person (e.g. mother, partner, friend) for follow-up. Screening and interventions were carried out in a private quiet area to ensure confidentiality and privacy for participants.
Participants were then screened for eligibility (structured questionnaire), after which they were randomly allocated to the brief intervention or to no intervention. If the participant was assigned to the brief intervention, the interviewer administered it. Arrangements were made for participants to be followed-up at 3 months and 12 months.
Assignment to brief intervention
Two hundred and seventy pieces of paper were divided into two equal groups: E (experimental) and C (control) and sealed in envelopes that were mixed and placed in a box, and kept in a locked on-site filing cabinet. To determine randomisation assignment of participants, interviewers opened the envelope on top of the pile after the participant had been screened.
Follow-up procedure
Participants were followed up 3 months and 12 months after recruitment, usually by the research nurse. The research nurse was not blind to the intervention status of the participant. Participants were administered the same survey instrument completed at baseline.
Where possible, the follow-up appointment was a face-to-face interview at the participant’s home. Where necessary, an alternative venue was arranged (e.g. a public place such as a coffee shop or public house). For participants that were difficult to track down, questionnaires were completed by telephone or, in some cases, mailed by (reply-paid) post. Appointment reminder letters were mailed to participants 1 month, and again 1 week, prior to their appointment. In addition, participants were usually telephoned the day prior to their appointment, to confirm the appointment details. Frequently, participants forgot or did not attend scheduled appointments, or had moved house. Several methods were used to make contact with these participants: telephone calls; letters; and unscheduled home visits. If contact with the participant did not occur within a week of the first follow-up, the secondary contact person was telephoned or visited. If the participant was not successfully contacted within 10 weeks of the originally scheduled follow-up appointment, they were considered to be lost to follow-up.
Measures
Survey data
The screening instrument took approximately 10–15 minutes to be administered and comprised items related to demographic information, alcohol use, and illicit substance use.
Alcohol use
Participants self-reported their alcohol consumption over a typical week prior to recruitment. For each day, the amount (e.g. pint; can size; double) and type of alcohol consumed by participants was recorded, in as much detail as possible (e.g. quantity and size of the container(s) from which alcohol was consumed); brand name (Stella lager; Jack Daniel’s; Scrumpy Jack cider), and alcohol concentration (where known). This information was later coded by the project manager into units of alcohol consumed, allowing computation of the following measures of alcohol consumption:
-
(a)
Total weekly units—number of units typically consumed by the participant over a 7-day period.
-
(b)
Number of drinking days in the past 3 months.
-
(c)
Frequency of drinking 8 or more standard units (less than weekly; weekly or more).
In order for the frequency of heavy episodic drinking to be assessed, participants were asked how frequently they consumed 8 or more standard units on one occasion. This item was derived from the FAST Alcohol Screening Test (Hodgson et al. 2002). Responses were categorised into two groups: less than weekly, or weekly/more frequently.
Alcohol Use Disorders Identification Test
The Alcohol Use Disorders Identification Test (AUDIT) is a ten-item screening instrument recommended by the World Health Organisation (Babor et al. 1992) for detecting hazardous/harmful levels of drinking, and alcohol dependence. AUDIT scores range from 0–40. WHO identifies scores of 8 or more as indicative of hazardous/harmful drinking and possibly of alcohol dependence (Babor et al. 1992). The AUDIT has been internationally validated for use in a number of settings.
Illicit substance use
Participants self-reported the frequency and amount of illicit substance use, including age at first use.
Attitudes to drinking
Attitude toward drinking behaviour was measured by the Readiness to Change Questionnaire (RCQ), a 12-item instrument that identifies ‘stage of change’ in relation to alcohol consumption (Heather and Rollnick 2000). The RCQ provides a short and convenient measure of a drinker’s stage of change for use in conjunction with brief, opportunistic interventions with excessive drinkers in medical and other settings. Allocation of participants to stage of change was achieved using the ‘refined’ method described by Heather and Rollnick (2000). This was performed at a later stage by the project manager and was independent of the screening process at the Magistrates’ court.
To assist with analyses of readiness to change drinking behaviour over time, a new variable was computed that described whether participants’ readiness to change drinking behaviour had increased, decreased, or stayed the same (relative to baseline). This was done at 3-month and 12-month follow-up. For instance, if a participant was in the ‘precontemplative’ stage at baseline, but in the ‘contemplative’ stage at 3-month follow-up, he would be allocated to the ‘positive’ category at 3-month follow-up.
Independent data
In addition to the survey data obtained at the screening interview (and both follow-up periods), two databases were accessed to provide objective, independent, measures of injury and offending by participants following their sentence.
Injury
A database of all attendances at accident and emergency (A&E) units in South Wales was accessed to determine whether participants had presented for treatment of an injury (violent, unintentional, or self-harm) between recruitment and the 12-month follow-up.
The proportion of participants in each group (intervention and control) who sustained an injury treated at an A&E unit in South Wales was calculated for each time period.
Offending
The Police National UK Crime Database was accessed to determine whether participants had been charged with an offence (violent; other) between recruitment and follow-up. To ensure that the data were as accurate as possible, they were obtained retrospectively, in relation to 3 months and 12 months after participants had been recruited (i.e. sentence date).
Intervention
The alcohol brief intervention was a manual-guided, tailored, intervention, based on the principles of motivational interviewing (Smith et al. 2003). Based on the feedback, responsibility, advice, menu, empathy, self-efficacy (FRAMES) methodology (Miller and Rollnick 1991), the intervention took approximately 15–20 minutes to be administered, and focused on a pamphlet that was designed specifically for the study, which was given to participants to take home. As suggested by the FRAMES methodology, the purpose of the brief intervention was to provide participants with information (about their level of drinking, what constitutes safe drinking levels, and the harms associated with drinking above these safe levels), as well as to encourage participants (in a non-judgemental way) to take responsibility for their drinking behaviour, and to provide the relevant tools to change their behaviour. The brief intervention in this study was modelled on previously used and validated brief interventions (Babor and Higgins-Biddle 2001; Miller and Rollnick 1991).
The research team were specifically trained in administration of the brief intervention. They were first familiarised with the theoretical underpinnings and rationale of the intervention, followed by a modelling of the intervention, then supervised role playing of intervention delivery. Researchers then watched the project manager model the intervention delivery to project participants in the Magistrates’ court and were then supervised by the project manager in delivery of the intervention to participants. Refresher sessions were held throughout the recruitment period to ensure consistency and accuracy in administration of the interventions.
Statistical analyses
A power calculation, based on a reduction in alcohol consumption by 20% of those in the intervention group (WHO 1996), demonstrated that a sample size of 200 was required (100 in the experimental group and 100 in the control group). This sample size would give at least 80% power to detect a difference between the groups of 20%.
Between-group differences at baseline were examined by analysis of variance (ANOVA) (for continuous variables) or chi-square analyses (categorical variables).
ANCOVA was used to examine between-group differences in alcohol measures at 3-month and 12-month follow-up. The corresponding baseline alcohol measure, and any other variables that differed between the groups at baseline, were entered as covariates in order to adjust appropriately for between-group differences in these measures (Newcombe 1998); 95% confidence intervals were calculated to examine the differences in the proportion of participants who reported drinking more than 8 standard units on a weekly or more frequent basis, and also to assess the proportion of participants who had re-offended or who had presented for treatment of an injury to an A&E unit in South Wales. Chi-square analyses were used to assess between-group differences in changes over time with respect to readiness to change drinking behaviour at 3-month and 12-month follow-up, relative to baseline.
Results
Participant selection
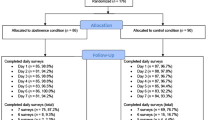
Figure 1 summarises the randomised controlled trial up to the conclusion of the study (12-months after sentence), in accord with the CONSORT statement (Moher et al. 2001). During the 12-month recruitment process, 1,857 men aged 16–35 years who lived within a 30-mile radius of Cardiff appeared at Cardiff Magistrates’ court charged with a violent offence. Over half of these offences were committed whilst the offender was intoxicated (n = 1,052; 56.6%). One-quarter of these alcohol-related offences remained ‘active’ in the judicial system at the end of the recruitment process (n = 267; 25.4%). Of the remaining men, 306 were ineligible for participation in the study: successful not guilty plea (n = 10); charge dismissed (n = 85); case transferred to Crown Court (n = 100); already recruited (n = 21); custodial sentence (n = 40); too violent (n = 10); previous or concurrent sex offence (n = 7); cognitive impairment (n = 13); hearing impairment (n = 1); non-English speaking (n = 8); intoxicated at court appearance (n = 2). Of the remaining 479 eligible participants, 269 were recruited (refused, n = 144; missed, n = 66), yielding a recruitment rate of 56.2%.
Flow diagram of participants’ involvement (CONSORT). Note: ‘Lost to follow-up’ refers to self-report data only (i.e. alcohol measures, RCQ responses). Objective measures (injury and re-offending rates) were obtained for all participants, regardless of whether they participated in the one-to-one follow-up (FU) sessions
Random allocation
Of 269 participants, 135 were randomly allocated to receive the alcohol brief intervention, and 134 participants received no intervention.
Follow-up rate
Two hundred and thirty-four (87%) participants were followed up at 3 months (FU1), and 202 were followed up at 12 months (FU2) (75.1%). There were no significant differences in follow-up rates as a function of intervention allocation:
-
FU1
cases = 88.1% vs controls = 83.6% (χ2 = 1.16; df = 1; P = 0.184)
-
FU2
cases = 74.8% vs controls = 71.6% (χ2 = 0.35; df = 1; P = 0.326)
It should be noted that ‘follow-up’ refers to survey data only. The majority of 3-month follow-ups (64.5%) occurred face-to-face with participants, although some follow-ups occurred by telephone (33.7%). Four participants self-completed the follow-up surveys and returned them by post. In contrast, the majority of 12-month follow-ups (57.9%) occurred by telephone, and 41.6% occurred face-to-face. Only one participant completed the 12-month follow-up by post. There were no differences in any of the survey measures (AUDIT; number of drinking days in the past 3 months; total weekly units; and stage of change) as a function of method of follow-up, at either 3-month or 12-month follow-up (p > 0.05). Independent data (injury and offending rates) were obtained from databases, and collection of these data was not affected by participation in follow-up interviews, regardless of follow-up method.
Sample characteristics
Demographic characteristics
The demographic characteristics of the sample are described in Table 2. Participants who were allocated to receive the intervention did not differ significantly from control participants in any of the demographic characteristics (P > 0.05), except education attainment. Participants in the intervention group were significantly less likely to report that they had attained their General Certificate of Secondary Education (GCSE) than were controls (χ2 = 6.22; df = 2; P = 0.045).
Substance use
There were no between-group differences in drug use patterns at baseline (P > 0.05). Over half of the sample reported using some type of illicit substance in the 3 months prior to recruitment (55.8%; n = 150). The three most frequently self-reported substances used in the 3 months prior to recruitment were: cannabis (n = 131); cocaine/crack (n = 35); and amphetamine (n = 33). Of those who reported using cannabis in the 3 months prior to recruitment, 40.2% (n = 53) reported using the substance on a daily basis; and 77.3% (n = 102) reported using the substance on at least a weekly basis. Of those who reported using amphetamine, 34.3% (n = 12) reported using the substance on only one occasion, and 42.9% (n = 15) reported using amphetamine once per month or more frequently. Over half (55.9%; n = 19) of the participants who reported using crack/cocaine reported using the substance on a monthly basis, and approximately one-quarter reported using the substance weekly (n = 23.5%; n = 8).
Baseline measures
Alcohol use
Mean AUDIT score for participants in the intervention group [20.19; standard error of the mean (SE) = 0.65] was significantly higher than for the control group (17.27; SE = 0.63). The majority of the sample (95.3%) scored > 8 (the cut-off point defined by WHO as indicative of hazardous/harmful drinking). There were no significant between-group differences in the proportion of participants scoring > 8 (intervention 94.8%; control 95.8%). One hundred and five participants (39.2%) scored > 20, the cut-off point defined by WHO as indicative of alcohol dependence. Significantly more participants in the intervention group scored > 20 than in the control group (χ2 = 8.28; df = 1; P = 0.004).
Total weekly standard units consumed did not differ significantly between groups at baseline (intervention mean = 63.36; SE = 4.9; control mean = 52.96; SE = 4.1; P = 0.11); however, participants in the intervention group reported significantly more drinking days (39 days) over the 3 months prior to receiving their sentence than control participants (P = 0.02). There were no significant between-group differences in the proportion of participants who reported drinking 8 or more standard units on a weekly or more frequent basis (intervention 82.2%; control 88.8%).
Evaluation of intervention
Alcohol consumption
Overall, significant reductions in three out of four measures of alcohol consumption from baseline to 3-month and 12-month follow-up were observed (P = 0.001; Figure 2). Whilst there was no significant reduction in weekly heavy episodic drinking between baseline and 3-month follow-up (baseline 85.5%; 3-month follow-up 86.7%; \(95\% {\text{CI}} = - 0.07, + 0.04\)), the proportion of participants at 12-month follow-up who reported weekly or more consumption of 8+ standard units had decreased significantly (12-month follow-up 78.2%; \(95\% {\text{CI}} = + 0.003, + 0.14\)). There were no significant between-group differences as a function of the intervention at 3-month follow-up (AUDIT, P = 0.18; weekly units, P = 0.39; number of drinking days, P = 0.94; weekly heavy episodic drinking, \(95\% {\text{CI}} = - 0.13, + 0.06\)), or 12-month follow-up (AUDIT, P = 0.61; weekly units, P = 0.79; number of drinking days, P = 0.95; weekly heavy episodic drinking, \(95\% {\text{CI}} = - 0.12, + 0.08\)), even after baseline differences on alcohol measures and education levels had been adjusted for in the analyses.
Injury
The proportion of intervention and control participants who had presented for treatment of an injury at an A&E unit in South Wales at 3-month and 12-month follow-up is shown in Table 3. Significant results are presented in bold type. Participants who had received an intervention were significantly less likely to present for treatment of an injury overall (27.4%) in the 12 months following their sentence than participants who had not received the intervention [39.6%; 95% confidence interval (CI) = −0.23, −0.009). There were no significant differences in rates of violent injury, unintentional injury, or self-harm, either at 3-month or 12-month follow-up.
Re-offending
Re-offending rates at 3-months and 12-months following sentencing (and recruitment) are shown in Table 3. Almost one-quarter of the sample (23.4%; n = 63) were charged with an offence in the 3 months following sentence, and 13% (n = 35) were charged with a violent offence. Almost half of the sample (47.2%; n = 127) were charged with an additional offence in the 12 months following their original sentence, and 16.7% were charged with a violent offence (n = 45). There were no between-group differences at either 3 months or 12 months after sentence.
Stage of change
Participants differed at baseline in their readiness to change in relation to drinking behaviour (χ2 = 19.38; df = 3; P < 0.001). Specifically, participants allocated to receive no intervention were more likely to demonstrate scores placing them in the precontemplative stage (i.e. not ready to reduce drinking), whereas participants allocated to receive the intervention were more evenly distributed across each stage of change (Table 4).
The data were examined so that it could be assessed whether there were significant differences in stage of change with respect to drinking behaviour over time. Almost one-third (n = 41; 30.5%) of the intervention group demonstrated an increase in their RTC drinking behaviour (e.g. a move from precontemplation to contemplation) at 3-month follow-up relative to baseline, compared with 16.4% (n = 22) of control participants (χ2 = 8.56; df = 2; P = 0.014). However, only 18.7% (n = 25) of the intervention group demonstrated an increase in RTC drinking behaviour at 12-month follow-up relative to baseline, compared with 52.5% (n = 70) of control participants (χ2 = 18.68; df = 2; P < 0.001).
Discussion
The principal finding of this study was that administration of an alcohol brief intervention to offenders in a Magistrates’ court immediately after sentencing did not reduce their alcohol consumption. Four other findings are noteworthy: (1) overall, participants in this study demonstrated a significant reduction in drinking (as observed on three out of the four measures of alcohol consumption) at 3-month follow-up, which persisted until 12-month follow-up; (2) participants who received the intervention were significantly less likely than control participants to be treated for an injury at an A&E unit in the 12-months following sentence; (3) there were no differences in re-offending rates between the intervention and control groups; (4) those in the brief intervention group were more likely than controls to change their attitude to drinking at 3-month follow-up, but this attitude change did not persist at 12-month follow-up. The initial intervention might, therefore, benefit from supplementation at 3 months to reinforce behavioural change.
More than half of the violent offence charges heard at Cardiff Magistrates’ court in the 12-month recruitment period were committed whilst the offender was intoxicated with alcohol. This is a conservative estimate of the true proportion of violent offences that were alcohol related, as it was only possible to recruit participants where information about intoxication at the time of offence was known (i.e. recorded by police or confirmed by the offender). These data confirm that screening for alcohol misuse should be a major concern in all Magistrates’ courts, at least in relation to violent offences, to inform decisions about sentencing and alcohol treatment orders. This group are erratic and unreliable users of health services and, therefore, may not contact alcohol misuse services unless this is part of the sentencing process.
In this study, administration of the brief intervention appears to have been successful in reducing objectively measured injury rates over time, but not in reducing alcohol consumption or re-offending rates. Monti et al. (1999) demonstrated that administration of a brief motivational intervention to 18–19 year olds who presented for treatment of an alcohol-related event at an Emergency Department significantly reduced a range of alcohol-related harms, such as drinking and driving, traffic violations, alcohol-related injuries, and alcohol-related problems at 6-month follow-up. Monti and colleagues did not observe a significant between-group difference in reduction of alcohol consumption, even though alcohol consumption did decrease in both groups. The finding in our study that there was a significant reduction in drinking among participants overall at both 3-month and 12-month follow-up indicates that being sentenced for a violent offence at a Magistrates’ court may, in itself, be effective in reducing alcohol misuse. This effect has been reported elsewhere in the literature. For instance, Gentilello et al. demonstrated that being injured whilst intoxicated prompted a reduction in alcohol consumption (1999). It is possible that in this study, being sentenced for an alcohol-related violent offence was sufficient to reduce alcohol consumption. Further research is required to test this hypothesis.
It is also possible that the screening process itself represents an intervention. Screening was detailed and sophisticated—participants were required to complete the ten-item AUDIT instrument on drinking behaviour, RCQ, and drug use. The initial impact of the screening may have been reinforced at 3-month and 12-month follow-up, when the same measures were completed. The screening process may institute changes in thinking, but the more cognitively involved processes required of the participant during the intervention may not be initiated because offenders’ minds are focused elsewhere (i.e. on their sentence and/or the ordeal of appearing in court). From these findings, it appears that, whilst a brief intervention in the immediate aftermath of sentencing may sensitise offenders to one of the causes of their offending, repetition or reinforcement during the first 3 months may also be necessary.
Further research is necessary to determine why the brief intervention was successful in reducing injury rates but not alcohol consumption or re-offending rates. It is possible that this finding is a function of the number of tests performed in the analyses. It is also possible that the brief intervention focused more on the consequences of drinking in terms of harms such as injury (to self and others) than on offending, or on other alcohol-related harms (social, personal, psychological, etc.). Focusing on injury may have been perceived as less confrontational by the interviewers.
Despite the finding in this study that the alcohol brief intervention was not effective at reducing alcohol consumption among violent offenders, administration of the brief intervention in this setting may still be useful in raising awareness that drinking behaviour is harmful. Participants who received an intervention increased their readiness to change drinking behaviour at 3 months in relation to those who did not receive an intervention. More than one-third of the sample scored > 20 in the AUDIT the cut-off point defined by WHO as indicative of alcohol dependence (Babor et al. 2001). Furthermore, significantly more participants in the intervention group scored > 20 than in the control group. According to the World Health Organisation (Babor and Higgins-Biddle 2001) AUDIT scores > 20 indicate the need for specialist referral, diagnostic evaluation and treatment—and not for brief interventions. In this study, logistical difficulties meant that AUDIT scores were not computed at the time of screening, so it was not possible to separate offenders who would benefit from administration of the alcohol brief intervention, or who should more appropriately be referred onwards for specialist treatment. However, WHO acknowledges that drinkers who score > 20 in the AUDIT may benefit from increased awareness that there is a need to change their drinking behaviour (Babor et al. 2001). Thus, even though a brief intervention administered to violent offenders immediately after sentencing may not be useful in reducing offenders’ alcohol consumption (or related harms, such as violent offending), there may be a role for the brief intervention in raising awareness that drinking behaviour is harmful. Further research on the effect of supplementation of the brief intervention is warranted.
Study limitations
Refusal rate
The refusal rate in this study was high - approximately one-quarter of eligible participants refused to participate in the study. Participating in this research often appeared unappealing to young men who had just been sentenced, due to lengthy delays often involved in court appearances.
Missed participants
A significant proportion (13.8%) of eligible participants were not approached for consent, due to a range of logistic difficulties. Fourteen courts were in operation at once, but a maximum of four researchers was available for recruitment at the court (usually only two). Substantial research resources were dedicated to the determination of whether offences had been committed when the offender was intoxicated. Frequently, there was no information about alcohol intoxication at the time of an offence. The CPS were dependent on police (and witness) reports for this information, and there was no consistency in recording. Some police officers recorded alcohol and substance use involvement as standard practice, whereas some officers recorded this information only when it appeared to be instrumental (e.g. in relation to a concurrent drink driving offence). Some officers did not refer to alcohol at all, even when it was clearly involved. Although defence solicitors were usually aware of alcohol involvement, they were sometimes reluctant to share this information with the research team, unless it formed part of the defence strategy.
Thirdly, approximately one-quarter of violent offence cases had not been concluded by the end of data collection. As directed by the protocol, these participants were excluded from the study. A suggestion for future randomised controlled trials of alcohol brief interventions in court settings is to expand the study to encompass those charged with offences (not necessarily sentenced), to allow offenders to be approached before sentence (e.g. at first appearance). Participants found not guilty could then be excluded at a later date.
Follow-up
Despite best efforts, 13% (n = 35) of offenders did not comply with first follow-up arrangements. This high rate of compliance represents a considerable achievement for this troubled population, which is relatively young, resistant to authority, antisocial and highly transient.
The majority of follow-up interviews were completed by the same person who recruited the participants (and performed the intervention, where applicable). It is possible that this may have biased the information obtained from participants at follow-up (alcohol measures; readiness to change drinking behaviour). No between-group differences were observed in relation to alcohol use, but participants in the intervention group were significantly more likely than those in the control group to report an increase in their readiness to change drinking behaviour. Ideally, this would have been avoided by blinding the researcher involved at the follow-up interview to the randomisation status of participants. However, in this study, one of the strategies employed to minimise loss to follow-up was to have the same person involved in recruitment and follow-up of participants. Whilst this strategy appears to have been successful in terms of reducing loss to follow-up, it is possible that the information obtained about readiness to change drinking behaviour at 3-month follow-up was biased. However, any possible bias in the data were no longer present by 12-month follow-up, as there were no between-group differences on this measure.
Randomisation
Some between-group differences were observed at baseline (education level, AUDIT, number of drinking days, and stage of change). It is possible that, despite the initial intensive training and ongoing refresher sessions, interviewers believed that they were providing assistance to participants who most needed help. Unfortunately, if it was prevalent, this perception was misguided. It is also possible that full interventions were not administered to participants who were perceived to be in the precontemplative stage of change, in the belief that motivating change in these participants would be difficult. While every effort was made throughout the recruitment phase of the project to monitor intervention delivery (regular, detailed briefing on the rationale underlying the procedure to the interviewing team; regular assessment that numbers of participants assigned to each group was equal), strict adherence to the protocol was in the hands of interviewers.
Conclusions
In summary, this study demonstrated that it is feasible to undertake a randomised controlled trial of an alcohol brief intervention in a judicial setting, albeit with considerable logistic and cultural difficulties. The results demonstrate that a standard alcohol brief intervention administered immediately after sentencing in a Magistrates’ court for a violent offence was not effective in reducing alcohol consumption or re-offending in the proceeding 12 months. However, it appears that the intervention may have been effective in reducing vulnerability to injury in offenders, and also improved readiness to reduce alcohol consumption in the first 3 months. These findings suggest that supplementation of alcohol brief intervention in the first 3 months after sentencing should be investigated, as should administration of the intervention at some other time during the first 3 months after sentencing (rather than immediately following sentencing). The results also indicate that both sentencing and screening for alcohol misuse may in themselves constitute effective interventions, and this should be further investigated. The high level of drinking reported by the majority of violent offenders in this study highlights the necessity for routine screening for alcohol misuse to be instituted as part of criminal proceedings. Investigation into interventions that may more appropriately address the high levels of alcohol consumption in this population is warranted.
References
Babor, T., De La Fuente, J., & Saunders, J. (1992). Programme on substance abuse: AUDIT, guidelines for use in primary care. World Health Organisation.
Babor, T. F., & Higgins-Biddle, J. C. (2001). Brief intervention for hazardous and harmful drinking: A manual for use in primary care. World Health Organisation. Department of Mental Health and Substance Dependence.
Babor, T. F., Higgins-Biddle, J. C., Saunders, J. G., & Monteiro, M. G., (2001). AUDIT: The alcohol use disorders identification test; guidelines for use in primary care (2nd ed.). World Health Organisation. Department of Mental Health and Substance Dependence.
Bien, T. H., Miller, W. R., & Tonigan, J. S. (1993). Brief interventions for those with alcohol problems: A review. Addiction, 88(3), 315–336.
Borges, G., Cherpitel, C., & Mittleman, M. (2004). Risk of injury after alcohol consumption: A case-crossover study in the emergency department. Social Science and Medicine, 58, 1191–2000.
Collins, J., & Messerschmidt, P. (1993). Epidemiology of alcohol related violence. Alcohol Health Research World, 17(2), 93–107.
Cordoba, R., Delgado, M. T., Pico, V., Altisent, R., Fores, C., Monreal, A., & Frisas, O. (1998). Effectiveness of brief intervention on non-dependent alcohol drinkers: A Spanish multi-centre study. Family Practice, 15(6), 562–568.
DiClemente, C., Prochaska, J., Fairhurst, S. K., Velicer, W., Velasquez, M. M., & Rossi, J. S. (1991). The process of smoking cessation: an analysis of the precontemplation, contemplation and preparation stages of change. Journal of Consulting and Clinical Psychology, 59, 295–304.
Dyehouse, J. M., & Sommers, M. S. (1998). Brief intervention after alcohol-related injuries. Nursing Clinics of North America, 33(1), 93.
Effective Health Care Review Team. (1993). Brief interventions and alcohol use: Are brief interventions effective in reducing harm associated with alcohol consumption? Effective Health Care Bulletin, 7, 1–13.
Emmen, M. J., Schippers, G. M., Bleijenberg, G., & Wollersheim, H. (2004). Effectiveness of opportunistic brief interventions for problem drinking in a general hospital setting: Systematic review. British Medical Journal, 328(7435), 318.
Fergusson, D., & Horwood, L. J. (2000). Alcohol abuse and crime: A fixed-effects regression analysis. Addiction, 95, 1525–1536.
Gentilello, L. F., Rivara, D., Donovan, G., Jurkovich, E., Durancing, C., Dunn, A., et al. (1999). Alcohol interventions in a trauma centre as a means of reducing the risk of injury recurrence. Annals of Surgery, 230, 473–483, Oct.
Heather, N., & Rollnick, S. (2000). Readiness to change questionnaire: User’s manual (revised version). Newcastle: Centre for Clinical Psychology and Healthcare Research, University of Northumbria.
Hodgson, R. J., Alwyn, T., John, B., Thom, B., & Smith, A. (2002). The FAST alcohol screening test. Alcohol and Alcoholism, 37, 61–66.
Miller, W. R., & Rollnick, S. (1991). Motivational interviewing: Preparing people to change addictive behaviour. New York: Guildford Press.
Moher, D., Schulz, K. F., & Altman, D. G. (2001). ‘The CONSORT statement: Revised recommendations for improving the quality of reports of parallel-group randomised trials’. Lancet, 357, 1191–1194.
Monteiro, M. G., & Gomel, M. (1998). World Health Organisation project on brief interventions for alcohol-related problems in primary health care settings. Journal of Substance Abuse, 3, 5–9.
Monti, P. M., Colby, S. M., Barnett, N. P., Spirito, A., Rohsenow, D. J., Myers, M., et al. (1999). Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology, 67(6):989–994.
Newcombe, R. G. (1998). Interval estimation for the difference between independent proportions: Comparison of eleven methods. Statistics in Medicine, 17, 873–890.
Richmond, R., Kehoe, L., Heather, N., & Wodak, A. (2000). Evaluation of a workplace brief intervention for excessive alcohol consumption: The Workscreen project. Preventive Medicine, 30(1), 51–63.
Rollnick, S., Heather, N., & Bell, A. (1992). Negotiating behaviour change in medical settings: the development of brief motivational interviewing. Journal of Mental Health, 1, 25–37.
Shepherd, J. P., Sutherland, I., & Newcombe, R. (2006). Relations between alcohol, violence and victimisation in adolescence. Journal of Adolescence, 28, 539–553.
Smith, A. J., Hodgson, R., Bridgeman, K., & Shepherd, J. (2003). A randomized controlled trial of a brief intervention after alcohol-related facial injury. Addiction, 98, 43–52.
Smith, A. J., Hodgson, R. J., & Shepherd, J. P. (2000). Reducing binge alcohol consumption in young men. London: AERC.
Wallace, P., Cutler, S., & Haines, A. (1988). A Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. British Medical Journal, 297, 663–668.
Werch, C. E., Carlson, J. M., Pappas, D. M., Edgemon, P., & DiClemente, C. C. (2000). Effects of a brief alcohol preventive intervention for youth attending school sports physical examinations. Substance Use and Misuse, 35(3), 421–432.
White, D., & Chen, P. (2002). Problem drinking and intimate partner violence. Journal of Studies on Alcohol, 63, 205–214.
Wilk, A., Jensen, N., & Havighurst, T. (1997). Meta-analysis of randomised control trials addressing brief interventions in heavy alcohol drinkers. Journal of General Internal Medicine, 12, 274–283.
World Health Organisation. (WHO). Brief Intervention Study Group. (1996). A cross-national trial of brief interventions with heavy drinkers. American Journal of Public Health, 86(7), 948–955.
Wright, S., Moran, L., Meyrick, M., O’Connor, R., & Touquet, R. (1998). Intervention by an alcohol health worker in an accident and emergency department. Alcohol and Alcoholism, 33(6), 651–656.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Watt, K., Shepherd, J. & Newcombe, R. Drunk and dangerous: a randomised controlled trial of alcohol brief intervention for violent offenders. J Exp Criminol 4, 1–19 (2008). https://doi.org/10.1007/s11292-007-9048-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11292-007-9048-7