Abstract
Background
Laparoscopic cholecystectomy is the procedure of choice for the treatment of symptomatic gallstones. Conversion to open surgery is reported to be necessary in 5–10% of cases. This study aimed to define those factors associated in English hospitals with the need to convert a laparoscopic cholecystectomy to an open procedure. These included patient-related and particularly nonpatient-related factors.
Methods
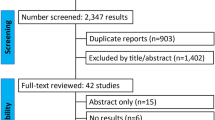
Using data derived from a national administrative database, Hospital Episode Statistics, patients undergoing cholecystectomy in acute National Health Service (NHS) hospitals in England during the financial years 2004–2006 were studied. The individual surgeon caseload and the hospital conversion rate were calculated using data from the first (baseline) year. Factors affecting the need for conversion were analyzed using data from the second (index) year.
Results
The study included 43,821 laparoscopic cholecystectomies undertaken from 2005 to 2006 in English hospitals. The overall conversion rate was 5.2%: 4.6% for elective procedures and 9.4% for emergency procedures. Patient-related factors that were good predictors of conversion included male sex, emergency admission, old age, and complicated gallstone disease (p < 0.001). Nonpatient-related factors that were good predictors of conversion included the laparoscopic cholecystectomy caseload of individual consultant surgeons and the overall hospital conversion rate in the previous year (all p < 0.001).
Conclusions
Conversion after laparoscopic cholecystectomy is less common as consultant caseload increases. This suggests that operation should be undertaken only by surgeons with an adequate caseload. There is a wide variation in conversion rates among hospitals. This has important implications for training as well as for the organization and accreditation of cholecystectomy services on a national basis.


Similar content being viewed by others
References
Muhe E (1986) The first cholecystectomy through the laparoscope. Langenbecks Arch Chir 396:804
NIH Consensus Conference (1993) Gallstones and laparoscopic cholecystectomy. JAMA 269:1018–1024
Wilson P, Leese T, Morgan WP, Kelly JF, Brigg JK (1991) Elective laparoscopic cholecystectomy for “all comers”. Lancet 338:795–797
Barkun JS, Barkun AN, Sampalis JS, Fried G, Taylor B, Wexler MJ, Goresky CA, Meakins JL (1992) Randomised controlled trial of laparoscopic versus mini cholecystectomy. The McGill Gallstone Treatment Group. Lancet 340:1116–1119
McMahon AJ, Russell IT, Baxter JN, Ross S, Anderson JR, Morran CG, Sunderland G, Galloway D, Ramsay G, O’Dwyer PJ (1994) Laparoscopic versus minilaparotomy cholecystectomy: a randomised trial. Lancet 343:135–138
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ (2006) Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev CD006231
Simopoulos C, Polychronidis A, Botaitis S, Perente S, Pitiakoudis M (2005) Laparoscopic cholecystectomy in obese patients. Obes Surg 15:243–246
Kama NA, Doganay M, Dolapci M, Reis E, Atli M, Kologlu M (2001) Risk factors resulting in conversion of laparoscopic cholecystectomy to open surgery. Surg Endosc 15:965–968
Alponat A, Kum CK, Koh BC, Rajnakova A, Goh PM (1997) Predictive factors for conversion of laparoscopic cholecystectomy. World J Surg 21:629–633
Ibrahim S, Hean TK, Ho LS, Ravintharan T, Chye TN, Chee CH (2006) Risk factors for conversion to open surgery in patients undergoing laparoscopic cholecystectomy. World J Surg 30:1698–1704
Livingston EH, Rege RV (2004) A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg 188:205–211
Tang B, Cuschieri A (2006) Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg 10:1081–1091
Wiebke EA, Pruitt AL, Howard TJ, Jacobson LE, Broadie TA, Goulet RJ Jr, Canal DF (1996) Conversion of laparoscopic to open cholecystectomy: an analysis of risk factors. Surg Endosc 10:742–745
Moore MJ, Bennett CL (1995) The learning curve for laparoscopic cholecystectomy. The Southern Surgeons Club. Am J Surg 170:55–59
Giger UF, Michel JM, Opitz I, Th Inderbitzin D, Kocher T, Krahenbuhl L (2006) Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22, 953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg 203:723–728
Kologlu M, Tutuncu T, Yuksek YN, Gozalan U, Daglar G, Kama NA (2004) Using a risk score for conversion from laparoscopic to open cholecystectomy in resident training. Surgery 135:282–287
Kama NA, Kologlu M, Doganay M, Reis E, Atli M, Dolapci M (2001) A risk score for conversion from laparoscopic to open cholecystectomy. Am J Surg 181:520–525
Lekawa M, Shapiro SJ, Gordon LA, Rothbart J, Hiatt JR (1995) The laparoscopic learning curve. Surg Laparosc Endosc 5:455–458
Riffenburgh RH (2006) Statistics in Medicine, 2nd edn. Elsevier Academic Press, Amsterdam
David GG, Al-Sarira AA, Willmott S, Deakin M, Corless DJ, Slavin JP (2008) Management of acute gallbladder disease in England. Br J Surg 95:472–476
Campbell SE, Campbell MK, Grimshaw JM, Walker AE (2001) A systematic review of discharge coding accuracy. J Public Health Med 23:205–211
Al-Sarira AA, David G, Willmott S, Slavin JP, Deakin M, Corless DJ (2007) Oesophagectomy practice and outcomes in England. Br J Surg 94:585–591
Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC (2006) Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg 93:844–853
NHS Institute for Innovation and Improvement (2006) Focus on Cholecystectomy. www.institute.nhs.uk/option,com_joomcart/Itemid,194/main_page,document_product_info/cPath,71/products_id,186.html
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ballal, M., David, G., Willmott, S. et al. Conversion after laparoscopic cholecystectomy in England. Surg Endosc 23, 2338–2344 (2009). https://doi.org/10.1007/s00464-009-0338-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0338-1