Abstract
Purpose
To evaluate the utility of the new Rebound tonometer for measuring intraocular pressure (IOP) in an unanesthetized eye; to test patient tolerance, measurement time, and accuracy compared with the Pulsair 3000 tonometer.
Methods
IOP was measured with the Rebound tonometer and the Pulsair 3000 tonometer without an anesthetic in 131 residents of two Finnish nursing homes. The measurement time and possible pain or discomfort experienced by the inhabitants was recorded.
Results
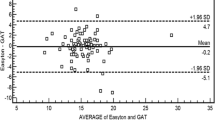
The mean differences in IOP readings between the two tonometers were 0.31 mmHg, SD 2.45 mmHg for the right eyes and 0.36 mmHg, SD 2.17 mmHg for the left eyes (P=0.28, multivariate analysis). The correlation constants between the tonometers were 0.84 (right eyes) and 0.80 (left eyes). The Pulsair 3000 caused more discomfort than the Rebound tonometer (36% vs 15%, P=0.01). With the Pulsair, 85%, and with the Rebound tonometer, 95% of the patients felt no pain (P= 0.14). Measurement of both eyes with the Rebound tonometer took less time (55±22 s vs 138±55 s, P<0.001). The mean difference was 82 s and the 95% confidence interval of the difference was 66–98 s.
Conclusion
Measurement of IOP with the Rebound tonometer without an anesthetic is a rapid and well-tolerated procedure. IOP readings of the two tonometers were within ±1 mmHg in 52.5% of the measurements and within ±2 mmHg in 71.7% of the measurements.



Similar content being viewed by others
References
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Dekking HM, Coster HD (1967) Dynamic tonometry. Ophthalmologica 154:59–74
Fisher JH, Watson PG, Spaeth G (1988) A new handheld air impulse tonometer. Eye 2:238–242
Friedenwald JS (1937) Contribution to the theory and practice of tonometry. Am J Ophthalmol 20:985–1024
Goldmann H, Schmidt TH (1957) Über Applanations-tonometrie. Ophthalmologica 134:221–242
Gräf M, Wassill H, Burkhard D (1995) Ein neues lageunabhängiges Tonometer (Proton) im Vergleich mit dem Goldmann-applanationstonometer. Klin Monatsbl Augenheilkd 206:255–261
Kocak I, Orgul S, Saruhan A, Haefliger I, Hendrickson P, Flammer J (1998) Measurement of intraocular pressure with a modern noncontact tonometer. Ophthalmologica 212:81–87
Kontiola AI (2000) A new induction-based impact method for measuring intraocular pressure. Acta Ophthalmol Scand 78:142–145
Kontiola AI, Goldblum D, Mittag T, Danias J (2001) The induction/impact tonometer: a new instrument to measure intraocular pressure (IOP) in the rat (RA). Exp Eye Res 73:781–785
Krakau CET (1970) A vibration tonometer. Ophthalmic Res 1:129–139
Leske MC (1983) The epidemiology of open-angle glaucoma: a review. Am J Epidemiol 118:166–191
Minckler DS, Baerveldt F, Heuer DK, Quillen-Thomas B, Walonker A, Weiner J (1987) Clinical evaluation of the Oculab Tonopen. Am J Ophthalmol 104:168–173
Parker VA, Herrtage J, Sarkies NJ (2001) Clinical comparison of the Keeler Pulsair 3000 with Goldmann applanation tonometry. Br J Ophthalmol 85:1303–1304
Ray WA, O’Day DM (1985) Statistical analysis of multi-eye data in ophthalmic research. Invest Ophthalmol Vis Sci 26:1186–1188
Ritch R, Lowe RF (1996) Angle-closure glaucoma: clinical types. In: Ritch R, Shields MP, Krupin T (eds) The glaucomas, vol 2. Mosby, St Louis, pp 821–840
Shields MB, Ritch R, Krupin T (1996) Classification of glaucomas. In: Ritch R, Shields MP, Krupin T. (eds) The glaucomas, vol 2. Mosby, St Louis, pp 717–725
Tangalos EG, Smith GE, Ivnik RJ, Petersen RC, Kokmen E, Kurland EG (1996) The Mini-Mental State Examination in general medical practice: clinical utility and acceptance. Mayo Clin Proc 71:829–837
Whitacre M, Stein R (1993) Sources of error with use of Goldmann-type tonometers. Surv Ophthalmol 38:1 1–30
Wright MM, Grajewski AL (1991) Measurement of intraocular pressure with a flat anterior chamber. Ophthalmology 98:12 1854–1857
Acknowledgements
This study was supported by TEKES (The Finnish National Technology Agency). The authors thank Jukka Ollgren, MSc., for his assistance with the statistical analyses and Jean Margaret Perttunen for revising their English.
Author information
Authors and Affiliations
Corresponding author
Additional information
Submitted as an abstract to the ARVO annual meeting, May 2002
Rights and permissions
About this article
Cite this article
Kontiola, A., Puska, P. Measuring intraocular pressure with the Pulsair 3000 and Rebound tonometers in elderly patients without an anesthetic. Graefe's Arch Clin Exp Ophthalmol 242, 3–7 (2004). https://doi.org/10.1007/s00417-003-0671-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-003-0671-3