Abstract
Rationale
Survivors of sepsis syndromes have poor outcomes for physical and cognitive function. No investigations of early physical rehabilitation in the intensive care unit have specifically targeted patients with sepsis syndromes.
Objective
To determine whether early physical rehabilitation improves physical function and associated outcomes in patients with sepsis syndromes.
Methods
Fifty critically ill adults admitted to a general intensive care unit with sepsis syndromes were recruited into a prospective double-blinded randomised controlled trial investigating early physical rehabilitation.
Measurements
Primary outcomes of physical function (acute care index of function) and self-reported health-related quality of life were recorded at ICU discharge and 6 months post-hospital discharge, respectively. Secondary measures included inflammatory biomarkers; Interleukin-6, Interleukin-10 and tumour necrosis factor-α, blood lactate, fat-free muscle mass, exercise capacity, muscle strength and anxiety.
Main results
A significant increase in patient self-reported physical function (81.8 ± 22.2 vs. 60.0 ± 29.4), p = 0.04) and physical role (61.4 ± 43.8 vs. 17.1 ± 34.4, p = 0.005) for the SF-36 at 6 months was found in the exercise group. Physical function scores were not significantly different between groups. Muscle strength scores were (51.9 ± 10.5 vs. 47.3 ± 13.6, p = 0.24) with the standard care mean Medical Research Council Muscle Score (MRC) <48/60. The mean change of Interleukin-10 increased and was significantly higher in the exercise group (1.8 pg/ml, 180 % vs. 0.9 pg/ml, 90 %, p = 0.04). There was no significant difference between groups for lactate, Interleukin-6, tumour necrosis factor-α, muscle strength, exercise capacity, fat-free mass or hospital anxiety.
Conclusion
Implementation of early physical rehabilitation can improve self-reported physical function and induce systemic anti-inflammatory effects.
Similar content being viewed by others
Introduction
Sepsis is defined as a powerful systemic response to severe infection. The incidence of severe sepsis is estimated to be between 50 and 100 cases per 100,000 people of the population in developed countries [1]. Associated with this disease burden is the cost of ongoing disability and loss of productivity post-critical illness. Patients with sepsis syndromes have significantly worse outcomes particularly in the physical and cognitive domains compared to age-matched normal [2] and other hospitalised patients [3]. A structured rehabilitation pathway is proposed to prevent these persistent long-term problems post-ICU discharge [4].
There is emerging evidence that early physical intervention in intensive care unit (ICU) can increase ventilator-free days, improve peripheral and respiratory strength, reduce length of ICU and hospital stay [5–7], and improve long-term physical [8]. There are no randomised prospective trials specifically on the effects of exercise in humans with sepsis. Animal models of sepsis have indicated that physical exercise post-sepsis increased bacterial clearance from blood and organs, decreased the release of pro- and anti-inflammatory cytokines and improved survival [9]. Additionally, there is evidence for preconditioning prior to the septic insult with less lung and distal organ injury occurring following sepsis [10]. Physical training prior to sepsis prevented atrophy, lipid peroxidation and protein oxidation in the skeletal muscles of septic rats [11].
Retrospective cohort analysis found that increased physiotherapy intervention in patients with sepsis resulted in less ICU mortality [12]. In the absence of prospective controlled trials specifically investigating early exercise intervention in sepsis, we aimed to investigate whether early physical rehabilitation improved physical function and self-reported health-related quality of life and associated secondary outcomes in patients with sepsis syndromes admitted to ICU.
Materials and methods
A prospective double-blinded randomised controlled trial [13] (ACTRN 12610000808044) was conducted at a single quaternary level, university-affiliated, general ICU at the Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia. Methodology for this trial is detailed in the protocol article [13]. The study was conducted according to CONSORT guidelines [14]. Participants, substitute decision makers, outcome assessors and health care personnel except treating therapists were blinded to group allocation.
Study population
Participants ≥18 years who remained mechanically ventilated ≥48 h and diagnosed with sepsis [15] (≥2 criteria of a systemic inflammatory response plus proven or strongly suspected infection), severe sepsis (sepsis plus organ failure), or septic shock (severe sepsis with hypotension not responding to fluid management) were enrolled. Patients with head injuries, burns, spinal injuries, or multiple fractured lower limbs and those with septic shock who were unresponsive to maximal treatment, moribund or had an expected mortality within 48 h were excluded. Written informed consent was obtained according to ethical guidelines. The study was approved by The Human Research Ethics Committee at Royal Brisbane and Women’s Hospital and the Medical Research Ethics Committee at The University of Queensland.
Participant age, sex, co-morbidities, admission diagnoses, acute physiological and chronic health evaluation (APACHE II) [16], Charlson comorbidity index (CCI) [17], sequential organ failure assessment (SOFA) [18], time on mechanical ventilation, ventilator-free days, length of ICU and hospital stay, readmissions to ICU and 90-day mortality in hospital or home were recorded. Enrolled participants were randomised into an intervention and standard care arm by computer generated randomisation http://www.randomization.com, using concealed allocation (Electronic supplementary material, ESM, Fig. S1).
ICU physical rehabilitation program
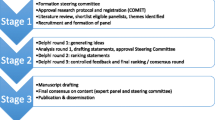
Participants in the intervention arm underwent individualised early targeted physical rehabilitation program prescribed by the ICU research physiotherapist for 30 min, one to two times daily until discharge from the ICU within 48 h of the diagnosis of sepsis (ESM, Table S1). Physical rehabilitation strategies included electrical muscle stimulation (EMS), passive range of motion, active range of motion, sitting out of bed, transfers, ambulation and other mobilisation techniques as appropriate. Targeted muscle groups for EMS were vastus medialis, vastus lateralis, tibialis anterior and brachioradialis. A frequency of 40–45 Hz at 20–25 mA with pulse duration at 400 μs of 12 s on and 6 s off was used. Participants in the standard care group received standard ICU care which included physical therapy strategies provided by the ICU physiotherapist. The physical rehabilitation received by both groups was recorded (Fig. 1). A safety audit was completed on patients in the intervention group during treatment.
Primary outcomes
Participants were assessed objectively for physical function using the acute care index of function (ACIF) [19] and self-reported health-related quality of life was measured by the SF-36 medical short-form (SF-36) by telephone at 6 months post-discharge from hospital [20].
Secondary outcomes
Secondary measures included exercise capacity using the physical functional ICU test (PFIT) [21], overall muscle strength using the Medical Research Council Muscle Score (MRC) [22] and psychological outcome using the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS) [23] on discharge from ICU. Pro- and anti-inflammatory activity were assessed objectively by monitoring cytokines; Interleukin-6 (IL-6), Interleukin-10 (IL-10) and tumour necrosis factor-α (TNF-α). Blood lactate (BL) concentration was assessed to determine whether exercise was inducing anaerobic glycolysis. Fat-free mass (FFM) was assessed for lean tissue muscle mass loss. Methodology for these measures is detailed in the protocol article [13]. Reliability, validity and responsiveness in the ICU [20, 24] and sepsis population [25, 26] for these measures are specified in the protocol article [13].
Sample size
Sample size calculations were based on physical function outcome of ACIF using previously published minimally clinical important differences and standard deviations 15.4 (SD 17) in an acute care trial [27]. A sample size of 35 per group (total 70) was calculated with an effect size of 0.7 and 90 % power with a type 1 error rate of 0.05 and 0.025 with Bonferroni adjustment.
Statistical analysis
Data were analysed using intention to treat. Non-normal data were log-transformed. Data were expressed as mean [standard deviation (SD)] or median [inter-quartile range (IQR)]. Single variables were compared using Student’s t test and dichotomous outcomes were analysed using a Chi-squared test or Fisher’s exact test as appropriate. A mixed method ANOVA managed missing data and was used to compare between/within groups at different time points. If the overall model was significant, multiple comparisons among pairs of means were analysed with post hoc Bonferroni correction of the significance level (p < 0.05).
Results
Fifty patients (5.2 % of those screened) were recruited with 26 and 24 participants randomised to the intervention and standard care group, respectively, during the period December 2010 to August 2012 (ESM, Fig. S1).
Demographics, ICU and hospital measures
The demographics of participants in the standard care and intervention groups are reported in Table 1. There were no significant baseline differences between the groups. There was no statistical significance between groups for duration of mechanical ventilation, ventilator-free days, ICU and hospital length of stay, ICU readmission, ICU and 90-day mortality and resuscitation (DNR) status (Table 1).
Adherence
There were no withdrawals during the conduct of the trial. All participants adhered and remained enrolled in the study for an average of 11.4 days. Figure 1 describes the details of the duration and number of episodes of exercise interventions administered to both groups.
Physical function
A total of 42 participants were assessed for physical function on discharge from ICU using a t test for independent groups. Eight patients were not suitable for assessment due to death in ICU (n = 4) and for the presence of delirium or reduced level of consciousness (n = 4). No differences were found in the physical function ACIF final scores (61.1 ± 33.1 vs. 55.0 ± 24.4, p = 0.45) and mobility scores (39.8 ± 38.2 vs. 34.5 ± 27.1, p = 0.67 (Table 2).
Health-related quality of life
Thirty participants completed the SF-36 quality of life survey at 6 months post-hospital discharge over the telephone. Sixteen patients were lost to further follow-up due to death (n = 12), non-contactable (n = 3) or readmitted to hospital (n = 1). An independent t test comparison between groups found that patients in the exercise group self-reported a significant quality of life improvement in the domains of physical function (81.8 ± 22.2 vs. 60.0 ± 29.4, p = 0.04) and physical role (61.4 ± 43.8 vs. 17.1 ± 34.4, p = 0.005), compared to those who received standard care. Patient report of emotional role (63.6 ± 40.7 vs. 33.3 ± 45.8, p = 0.08), vitality (45.9 ± 12.0 vs. 39.2 ± 7.7, p = 0.07) and general health (50.5 ± 11.9 vs. 41.8 ± 11.3, p = 0.06) all showed a trend towards statistical significance. Early rehabilitation did not impact on reports of bodily pain, social functioning or mental health (Table 3).
Hospital anxiety
Thirty-five participants were able to complete the HAS assessment at ICU discharge. Fifteen participants were not successful in testing due to death (n = 4), inability to converse or delirium (n = 11). A t test for independent groups found no statistically significant changes between mean scores with ICU early exercise; however, a Chi-squared crosstabs found that there was a trend for a greater number of patients in the intervention group having low levels of anxiety (25 vs. 14 %, p = 0.09) (Table 3).
Exercise capacity and muscle strength
A total of 42 participants were tested for exercise capacity and overall muscle strength at ICU discharge. No differences were found in ICU exercise capacity using the interval PFIT score (5.6 ± 2.1 vs. 5.4 ± 1.7, p = 0.61). Although not statistically significant, the standard care group recorded a mean MRC score of less than 48/60 for the MRC scale consistent with the criteria for ICUAW [28] (Table 2).
Inflammatory biomarkers
Interleukin-6
The pro-inflammatory cytokine; IL-6 was measured on days 1, 3, 5, and 7 upon initiation of the trial and at ICU discharge. A reduction in IL-6 mean scores was observed in the intervention group pre- and post-exercise across days 1, 3, 5 and 7 but no statistically significant differences were found between groups. There was a trend towards significance for mean change from baseline to ICU discharge where the decrease was greater (5.2 pg/ml, 55 % vs. 20.4 pg/ml 120 %, p = 0.07) (ESM, Table S2) in the intervention group with a mixed model ANOVA (Fig. 2).
Interleukin-10
The anti-inflammatory cytokine, Interleukin-10, was measured on days 1, 3, 5, and 7 and at ICU discharge. Overall mean change of IL-10 from baseline to ICU discharge was significantly higher in the intervention group (1.8 pg/ml, 180 % vs. 0.9 pg/ml, 90 %, p = 0.04) (ESM, Table S2) than in the standard care group (Fig. 2).
Tumour necrosis factor-α
The pro-inflammatory cytokine, tumour necrosis factor-α, was also measured on days 1, 3, 5, and 7 and at ICU discharge. There were statistically significant findings between groups from baseline to ICU discharge with a greater percentage decrease in the standard care group (2.5 pg/ml, 100 % vs. 2.5 pg/ml, 75 %, p < 0.01) (Table S2) (Fig. 2).
Fat-free mass
Percentage fat-free mass was measured at recruitment (n = 44), week 1 (n = 32) and at ICU discharge (n = 17). Six patients were ineligible for the use of BIS at recruitment due to missing a limb, presence of metal implants or peripheral or generalised oedema. Fat-free mass increment at week 1 was noted but the groups were not significantly different (ESM, Fig. S2a). Percentage changes in fat-free mass showed increments in both groups at week 1 and reductions at ICU discharge from baseline (4.4 vs. 2.5 %, −1.2 vs. −5.1 %, p = 0.93) (ESM, Fig. S2b).
Safety measures
Blood lactate
Blood lactate concentrations were determined pre- and post-exercise as a safety marker for exercise. Lactate showed significant effects for time and decreased in both groups over the course of the week (p = 0.04). It did not increase post-exercise in the intervention group (ESM, Table S3).
Vital signs
As a further measure of safety, arterial blood pressure, heart rate, respiratory rate and oxygen saturation were monitored during all sessions of exercise. There were pre-determined alterations which would define an adverse event [13]. No session of exercise resulted in an adverse event.
Discussion
Early physical rehabilitation for critically ill patients with sepsis resulted in a significant health-related quality of life improvement in self-reported physical function and physical role at 6 months post-hospital discharge. In addition, there were trends towards improvement in emotional role, vitality and general health and less anxiety on ICU discharge. There were significantly larger increases in the early exercise group for the anti-inflammatory cytokine IL-10. There were no significant effects on physical function, exercise capacity or fat-free mass on discharge from intensive care.
Previous studies in intensive care have reported positive outcomes for general patients with a combined intervention of early rehabilitation [5, 29, 30]. A number of studies have not shown a difference between groups [31, 32], but it can be noted that the group of “standard care” received a high level of exercise due to existing local practices. Our study differed, in that we investigated a discrete group of patients with sepsis syndromes. This group have been shown to have worse physical and cognitive deficits than other diagnostic groups in ICU, so there may have been more potential for improvement [2, 3]. Additionally, we provided intervention such as EMS and passive exercise in the early stage when patients were sedated and unable to participate in active movement. The dose of early physical rehabilitation provided in this trial, i.e. 30 min a day, is a feasible treatment to be delivered in typical intensive care settings.
Specific studies have been undertaken utilising EMS with contradictory outcomes [6] with preservation of muscle mass found in long-stay ICU patients. Studies that targeted patients with sepsis [33, 34] did not find preservation of their muscle mass. However, this may have occurred as sepsis is a systemic inflammatory disease and exercise lowers overall inflammatory activity, hence exercising one part of the body with the other leg serving as a control may not be effective.
Our study included a high proportion of those receiving EMS or passive exercise when patients were high acuity, or when sedation produced a decreased level of co-operation. This was more common early in the admission; however, some patients deteriorated and passive manoeuvres were substituted for more active forms of exercise. We are of the opinion that providing some form of exercise at these stages as well as more active interventions produced a higher level of physical function overall in the later stages as determined from the improved HrQOL. Recent studies using a deeply sedated and mechanically ventilated experimental ICU rat model [35, 36] found preservation of muscle mass and muscle force generation after passive mechanical loading.
In addition, a number of factors in sepsis predispose towards greater potential loss of muscle mass and force which were reported as secondary measures in this study. The pro-inflammatory cytokines; Interleukin-6 and tumour necrosis factor-α, are involved in muscle degradation, myocyte degeneration and muscle atrophy, inhibition of protein synthesis and apoptosis [37–41]. Significant muscle wasting from bed rest occurs early in critical illness [42], which results from increased proteolytic degradation as well as decreased protein synthesis. The anti-inflammatory cytokine, Interleukin-10 (IL-10), is considered to inhibit proteolysis [43]. In this study, the rate of increase of IL-10 was twice the rate in the exercise group. Although novel and preliminary, this may contribute to some pertinent information relating to the mechanism underlying the effect of exercise on the systemic inflammatory response.
The ACIF score was an objective measurement used to assess basic physical function change at ICU discharge (short term) and the SF-36 assessed self-reported quality of life at 6 months (long term) by telephone. As many subjects were discharged to rural areas, a remote form of assessment was required at 6 months during which ICU survivors may exhibit physical- and emotional-related difficulties [44]. Although the SF-36 indicated increased self-reported physical function, we could not conclude that it directly translated into demonstrably improved physical function, as a physical function assessment or muscle strength assessment was not performed at 6 months to confirm this. However, a self-perception of improved physical function would assist in increasing participation and aid recovery as per the international classification of functioning, disability and health (ICF) [45].
Previous studies have found a correlation between strength and function [26, 46] in general ICU patients; however, the timing of the assessment in our study, i.e. on discharge from ICU, may have influenced the results. The blinded assessor reported that, although able to complete a simple strength assessment, patients were not able to complete transfers due to problems with initiation of movements. Baldwin et al. [47] noted the same difficulties in a similar population. Deficits in motor control neural programming may have resulted in adequate strength not translating to efficient motor functioning, and repeating the tests at a later date may have shown significance between groups [48]. Additionally, we did not see a significant difference in exercise capacity (PFIT) consistent with the limitations of this ICU exercise capacity test [49].
Patients post-sepsis have been reported to have problems with cognition, anxiety, and post-traumatic syndromes as well as physical problems. We did not specifically address these in this study. However, there was a trend towards fewer patients in the intervention group reporting severe anxiety and a trend towards a higher score in the emotional role (SF-36). Exercise has frequently been reported to lessen anxiety [50–52]. A recent study has combined both physical and cognitive interventions with no differences found [32]. Although early cognitive intervention may aid in improving post-critical illness outcomes [53], larger numbers may be required to demonstrate an effect.
Blood lactate concentration was used in the study as a safety measure to ensure that exercise did not result in clinically significant anaerobic glycolysis. Pilot data of other secondary outcome measures of mitochondrial DNA, muscle oxygenation and microcirculation obtained during this main randomised trial will be reported in future manuscripts.
Limitations
This original study has some limitations. Firstly, the expected sample size was not reached due to time logistics for study completion. In addition, some bias may have been unavoidable in the overall analysis of the HrQOL outcomes due to the small sample available at 6 months from early deaths. Basic physical function as measured by the ACIF score was not assessed at the long-term stage. Hospital readmission was not monitored, and there was also a lack of baseline data on physical function, muscle strength and exercise capacity as is the nature of a critical care admission.
Conclusion
Early ICU exercise can moderate the detrimental effects of sepsis. It can improve self-reported quality of life in the physical domains and induce anti-inflammatory effects. Further research is required to look at the detailed mechanisms behind these effects in order to refine and tailor approaches to physical rehabilitation in the critically ill.
References
Danai P, Martin GS (2005) Epidemiology of sepsis: recent advances. Curr Infect Dis Rep 7:329–334
Hofhuis JG, Spronk PE, van Stel HF, Schrijvers AJ, Rommes JH, Bakker J (2008) The impact of severe sepsis on health-related quality of life: a long-term follow-up study. Anesth Analg 107:1957–1964
Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 304:1787–1794
Jones C (2013) What’s new on the post-ICU burden for patients and relatives? Intensive Care Med 39:1832–1835
Kayambu G, Boots RJ, Paratz JD (2013) Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med 41:1543–1554
Parry S, Berney S, Granger C, Koopman R, El-Ansary D, Denehy L (2013) Electrical muscle stimulation in the intensive care setting: a systematic review. Crit Care Med 41:2406–2418
Maffiuletti NA, Roig M, Karatzanos E, Nanas S (2013) Neuromuscular electrical stimulation for preventing skeletal-muscle weakness and wasting in critically ill patients: a systematic review. BMC Med. doi:10.1186/1741-7015-1111-1137
Calvo-Ayala E, Khan BA, Farber MO, Ely E, Boustani MA (2013) Interventions to improve the physical function of ICU survivors: a systematic review. Chest 144:1469–1480
Sossdorf M, Fischer J, Meyer S, Dahlke K, Wissuwa B, Seidel C, Schrepper A, Bockmeyer C, Lupp A, Neugebauer S, Schmerler D, Rodel J, Claus R, Otto G (2013) Physical exercise induces specific adaptations resulting in reduced organ injury and mortality during severe polymicrobial sepsis. Crit Care Med 41:E246–E255
de Araujo CC, Silva JD, Samary CS, Guimaraes IH, Marques PS, Oliveira GP, do Carmo LG, Goldenberg RC, Bakker-Abreu I, Diaz Bl, Rocha NN, Capelozzi Vl, Pelosi P, Rocco PR (2012) Regular and moderate exercise before experimental sepsis reduces the risk of lung and distal organ injury. J Appl Physiol 112:1206–1214
Coelho CW, Jannig PR, Souza AB, Fronza HJ, Westphal GA, Petronilho F, Constantino L, Dal-Pizzol F, Ferreira GK, Streck EE, Silva E (2013) Exercise training prevents skeletal muscle damage in an experimental sepsis model. Clinics 68:107–114
Sossdorf M, Otto GP, Menge K, Claus R, Losche W, Kabisch B, Kohl M, Smolenski UC, Schlattmann P, Reinhart K, Winning J (2013) Potential effect of physiotherapeutic treatment on mortality rate in patients with severe sepsis and septic shock: a retrospective cohort analysis. J Crit Care 28:954–958
Kayambu G, Boots RJ, Paratz JD (2011) Early rehabilitation in sepsis: a prospective randomised controlled trial investigating functional and physiological outcomes : the i-PERFORM trial (protocol article). BMC Anesthesiol. doi:10.1186/1471-2253-1111-1121
Schulz KF, Altman DG, Moher D (2011) CONSORT 2010 statement:updated guidelines for reporting parallel group randomised trials. Int J Surg 9:672–677
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT et al (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med 36:1394–1396
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Charlson ME, Pompe P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Vincent JLMR, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (sepsis related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
Van Dillen LR, Roach KE (1988) Reliability and validity of the acute care index of function for patients with neurologic impairment. Phys Ther 68:1098–1101
Contopoulos-Ioannidis DG, Karvouni A, Kouri I, Ioannidis JP (2009) Reporting and interpretation of SF-36 outcomes in randomised trials: systematic review. BMJ. doi:10.1136/bmj.a3006
Skinner EH, Berny S, Warrillow S, Denehy L (2009) Development of a physical function outcome measure (PFIT) and a pilot exercise training protocol for use in intensive care. Crit Care Resusc 11:110–115
De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Zaleski ID, Boussarsar M, Charles C, Renaud E, Mesrati F, Carlet J, Raphae JC, Outin H, Bastuji-Garin S (2002) Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 288:2859–2867
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Eddleston JM, White P, Guthrie E (2000) Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med 28:2293–2299
Heyland DK, Hopman W, Coo H, Tranmer J, McColl MA (2000) Long term health related quality of life in survivors of sepsis. Short form 36: a valid and reliable measure of health related quality of life. Crit Care Med 28:3599–3605
Nordon-Craft A, Schenkman M, Edbrooke L, Malone D, Moss M, Denehy L (2014) The physical function intensive care test: implementation in survivors of critical illness. Phys Ther 94:1499–1507
Roach KE, Ally D, Finnerty B, Watkins D, Litwin BA, Janz-Hoover B, Watson T, Curtis KA (1998) The relationship between duration of physical therapy services in the acute care setting and change in functional status in patients with lower extremity orthopaedic problems. Phys Ther 78:19–24
Brunello AG, Haenggi M, Wigger O, Porta F, Takala J, Jakob SM (2010) Usefulness of a clinical diagnosis of ICU-acquired paresis to predict outcome in patients with SIRS and acute respiratory failure. Intensive Care Med 36:66–74
Burtin C, Langer D, Troosters T, Hermans G, Decramer M (2009) Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med 37:2499–2505
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, Mccallister KE, Hall JB, Kress JP (2009) Early physical and occupational therapy in mechanically ventilated critically ill patients : a randomised controlled trial. Lancet 373:1874–1882
Denehy L, Skinner EH, Edbrooke L, Haines K, Warrillow S, Hawthorne G, Gough K, Hoorn SV, Morris ME, Berney S (2013) Exercise rehabilitation for patients with critical illness: a randomized controlled trial with 12 months follow up. Crit Care. doi:10.1186/cc12835
Brummel NE, Girard TD, Ely EW, Pandharipande PP, Morandi A, Hughes CG, Graves AJ, Shintani A, Murphy E, Work B, Pun BT, Boehm L, Gill TM, Dittus RS, Jackson JC (2014) Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: the activity and cognitive therapy in ICU (ACT-ICU) trial. Intensive Care Med 40:370–379
Poulsen JB, Moller K, Jensen CV, Weisdorf S, Kehlet H, Perner A (2011) Effect of transcutaneous electrical muscle stimulation on muscle volume in patients with septic shock. Crit Care Med 39:456–461
Rodriguez PO, Setten M, Maskin LP, Bonelli I, Vidomlansky SR, Attie S, Sl Frosiani, Kozima S, Valentini R (2012) Muscle weakness in septic patients requiring mechanical ventilation: protective effect of transcutaneous neuromuscular electrical stimulation. J Crit Care 27:311–318
Llano-Diez M, Renaud G, Andersson M, Marrero H, Cacciani N, Engquist H, Corpeno R, Artemenko K, Bergquist J, Larsson L (2012) Mechanisms underlying ICU muscle wasting and effects of passive mechanical loading. Crit Care. doi:10.1186/cc11841
Renaud G, Llano-Diez M, Ravara B, Gorza L, Feng HZ, Jin JP, Cacciani N, Gustafson AM, Ochala J, Corpeno R, Li M, Hedstrom Y, Ford GC, Nair KS, Larsson L (2013) Sparing of muscle mass and function by passive loading in an experimental intensive care unit model. J Physiol 1:1385–1402
Sharma R, Anker S (2002) Cytokines, apoptosis and cachexia: the potential for TNF antagonism. Int J Cardiol 85:161–171
Sandi M (2002) Apoptotic signaling in skeletal muscle fibres during atrophy. Curr Opin Clin Nutr Metab Care 5:249–253
Haddad F, Zaldivar F, Cooper D, Adams GR (2005) IL-6-induced skeletal muscle atrophy. J Appl Physiol 98:911–917
Dupont-Versteegden EE (2006) Apoptosis in skeletal muscle and its relevance to atrophy. World J Gastroenterol 12:7463–7466
Bonaldo P, Sandri M (2013) Cellular and molecular mechanisms of muscle atrophy. Dis Model Mech 6:25–39
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Phadke R, Dew T, Sidhu PS, Velloso C, Seymour J, Agley CC, Selby A, Limb M, Edwards LM, Smith K, Rowlerson A, Rennie MJ, Moxham J et al (2013) Acute skeletal muscle wasting in critical illness. JAMA 310:1591–1600
Oberholzer A, Oberholzer C, Moldawer LL (2002) IL-10: a complex role in the pathogenesis of sepsis syndromes and its potential as an anti-inflammatory drug. Crit Care Med 30:S58–S63
Schmidt M, Zogheib E, Roze H, Repesse X, Lebreton G, Luyt CE, Trouillet JL, Brechot N, Nieszkowska A, Dupont H, Ouattara A, Leprince P, Chastre J, Combes A (2013) The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med 39:1704–1713
Rauch A, Cieza A, Stucki G (2008) How to apply the international classification of functioning, disability and health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabil Med 44:329–342
Lisa JB, Kate F, Lara E, Selina MP, Rachel C, Thomas R, Susan CB, Linda D (2014) Low physical activity levels and poorer muscle strength are associated with reduced physical function at intensive care unit discharge: an observational study. In: C44 critical illness predictors and outcomes. American Thoracic Society 2014 International Conference, May 16-21, 2014, San Diego, A4543–A4543. doi:10.1164/ajrccm-conference.2014.189.1_MeetingAbstracts.A4543
Baldwin CE, Bersten AD (2014) Alterations in respiratory and limb muscle strength and size in patients with sepsis who are mechanically ventilated. Phys Ther 94:68–82
Huang CH, Martin AD, Davenport PW (2003) Effect of inspiratory muscle strength training on inspiratory motor drive and RREP early peak components. J Appl Physiol 94:462–468
Denehy L, de Morton NA, Skinner EH, Edbrooke L, Haines K, Warrillow S, Berney S (2013) A physical function test for use in the intensive care unit: validity, responsiveness, and predictive utility of the physical function ICU test (scored). Phys Ther 93:1636–1645
Merom D, Phongsavan P, Wagner R, Chey T, Marnane C, Steel Z, Silove D, Bauman A (2008) Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders—a pilot group randomized trial. J Anxiety Disord 22:959–968
Broman-Fulks JJ, Storey K (2008) Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety Stress Coping 21:117–128
Herring MP, Ml Jacob, Suveg C, Dishman R, O’Connor PJ (2012) Feasibility of exercise training for the short-term treatment of generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom 81:21–28
Hopkins RO (2014) Early cognitive and physical rehabilitation: one step towards improving post-critical illness outcomes. Intensive Care Med 40:442–444
Acknowledgments
This project was funded by Intensive Care Foundation. Ms. Kayambu was supported by a Postgraduate Award from Singapore. This project was supported in kind by the Burns, Trauma and Critical Care Research Centre. We would like to thank the Royal Brisbane and Women’s Hospital for the support of facilities to conduct this research.
Conflicts of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Early physical rehabilitation in intensive care can both improve self-reported physical function and induce systemic anti-inflammatory effects in patients with sepsis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kayambu, G., Boots, R. & Paratz, J. Early physical rehabilitation in intensive care patients with sepsis syndromes: a pilot randomised controlled trial. Intensive Care Med 41, 865–874 (2015). https://doi.org/10.1007/s00134-015-3763-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3763-8