Abstract
Purpose
Regional citrate anticoagulation (RCA) is an attractive anticoagulation mode in continuous renal replacement therapy (CRRT) because it restricts the anticoagulatory effect to the extracorporeal circuit. In recent years, several randomized controlled trials have been conducted to investigate its superiority over other anticoagulation modes. Thus, we performed a systematic review of available evidence on the efficacy and safety of RCA.
Methods
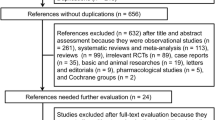
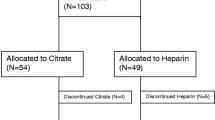
A systematic review of randomized controlled trials investigating the efficacy and safety of RCA was performed. PubMed, Current Contents, CINAHL, and EMBASE databases were searched to identify relevance articles. Data on circuit life span, bleeding events, metabolic derangement, and mortality were abstracted. Mean difference was used for continuous variables, and risk ratio was used for binomial variables. The random effects or fixed effect model was used to combine these data according to heterogeneity. The software Review Manager 5.1 was used for the meta-analysis.
Results
Six studies met our inclusion criteria, which involved a total of 658 circuits. In these six studies patients with liver failure or a high risk of bleeding were excluded. The circuit life span in the RCA group was significantly longer than that in the control group, with a mean difference of 23.03 h (95% CI 0.45–45.61 h). RCA was able to reduce the risk of bleeding, with a risk ratio of 0.28 (95% CI 0.15–0.50). Metabolic stability (electrolyte and acid–base stabilities) in performing RCA was comparable to that in other anticoagulation modes, and metabolic derangements (hypernatremia, metabolic alkalosis, and hypocalcemia) could be easily controlled without significant clinical consequences. Two studies compared mortality rate between RCA and control groups, with one reported similar mortality rate and the other reported superiority of RCA over the control group (hazards ratio 0.7).
Conclusions
RCA is effective in maintaining circuit patency and reducing the risk of bleeding, and thus can be recommended for CRRT if and when metabolic monitoring is adequate and the protocol is followed. However, the safety of citrate in patients with liver failure cannot be concluded from current analysis. The metabolic stability can be easily controlled during RCA. Survival benefit from RCA is still controversial due to limited evidence.



Similar content being viewed by others
References
Uchino S, Fealy N, Baldwin I, Morimatsu H, Bellomo R (2003) Continuous is not continuous: the incidence and impact of circuit “down-time” on uraemic control during continuous veno-venous haemofiltration. Intensive Care Med 29:575–578
Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten H, Ronco C, Kellum JA (2007) Continuous renal replacement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med 33:1563–1570
Tsang DJ, Tuckfield A, Macisaac CM (2011) Audit of safety and quality of the use of enoxaparin for anticoagulation in continuous renal replacement therapy. Crit Care Resusc 13:24–27
Gajra A, Vajpayee N, Smith A, Poiesz BJ, Narsipur S (2007) Lepirudin for anticoagulation in patients with heparin-induced thrombocytopenia treated with continuous renal replacement therapy. Am J Hematol 82:391–393
Link A, Girndt M, Selejan S, Mathes A, Böhm M, Rensing H (2009) Argatroban for anticoagulation in continuous renal replacement therapy. Crit Care Med 37:105–110
Windeløv NA, Ostrowski SR, Perner A, Johansson PI (2010) Transfusion requirements and clinical outcome in intensive care patients receiving continuous renal replacement therapy: comparison of prostacyclin vs. heparin prefilter administration. Blood Coagul Fibrinolysis 21:414–419
Pinnick RV, Wiegmann TB, Diederich DA (1983) Regional citrate anticoagulation for hemodialysis in the patient at high risk for bleeding. N Engl J Med 308:258–261
Aman J, Nurmohamed SA, Vervloet MG, Groeneveld AB (2010) Metabolic effects of citrate- vs bicarbonate-based substitution fluid in continuous venovenous hemofiltration: a prospective sequential cohort study. J Crit Care 25:120–127
Tillman J (2009) Heparin versus citrate for anticoagulation in critically ill patients treated with continuous renal replacement therapy. Nurs Crit Care 14:191–199
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Nurmohamed SA, Vervloet MG, Girbes AR, Ter Wee PM, Groeneveld AB (2007) Continuous venovenous hemofiltration with or without predilution regional citrate anticoagulation: a prospective study. Blood Purif 25:316–323
Fabbri LP, Nucera M, Al Malyan M, Becchi C (2010) Regional anticoagulation and antiaggregation for CVVH in critically ill patients: a prospective, randomized, controlled pilot study. Acta Anaesthesiol Scand 54:92–97
Park JS, Kim GH, Kang CM, Lee CH (2011) Regional anticoagulation with citrate is superior to systemic anticoagulation with heparin in critically ill patients undergoing continuous venovenous hemodiafiltration. Korean J Intern Med 26:68–75
Betjes MG, van Oosterom D, van Agteren M, van de Wetering J (2007) Regional citrate versus heparin anticoagulation during venovenous hemofiltration in patients at low risk for bleeding: similar hemofilter survival but significantly less bleeding. J Nephrol 20:602–608
Fealy N, Baldwin I, Johnstone M, Egi M, Bellomo R (2007) A pilot randomized controlled crossover study comparing regional heparinization to regional citrate anticoagulation for continuous venovenous hemofiltration. Int J Artif Organs 30:301–307
Hetzel GR, Schmitz M, Wissing H, Ries W, Schott G, Heering PJ, Isgro F, Kribben A, Himmele R, Grabensee B, Rump LC (2011) Regional citrate versus systemic heparin for anticoagulation in critically ill patients on continuous venovenous haemofiltration: a prospective randomized multicentre trial. Nephrol Dial Transplant 26:232–239
Kutsogiannis DJ, Gibney RT, Stollery D, Gao J (2005) Regional citrate versus systemic heparin anticoagulation for continuous renal replacement in critically ill patients. Kidney Int 67:2361–2367
Monchi M, Berghmans D, Ledoux D, Canivet JL, Dubois B, Damas P (2004) Citrate vs. heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med 30:260–265
Oudemans-van Straaten HM, Bosman RJ, Koopmans M, van der Voort PH, Wester JP, van der Spoel JI, Dijksman LM, Zandstra DF (2009) Citrate anticoagulation for continuous venovenous hemofiltration. Crit Care Med 37:545–552
Jackson SP, Nesbitt WS, Kulkarni S (2003) Signaling events underlying thrombus formation. J Thromb Haemost 1:1602–1612
Burry LD, Tung DD, Hallett D, Bailie T, Carvalhana V, Lee D, Ramganesh S, Richardson R, Mehta S, Lapinsky SE (2009) Regional citrate anticoagulation for PrismaFlex continuous renal replacement therapy. Ann Pharmacother 43:1419–1425
Bos JC, Grooteman MP, van Houte AJ, Schoorl M, van Limbeek J, Nubé MJ (1997) Low polymorphonuclear cell degranulation during citrate anticoagulation: a comparison between citrate and heparin dialysis. Nephrol Dial Transplant 12:1387–1393
Böhler J, Schollmeyer P, Dressel B, Dobos G, Hörl WH (1996) Reduction of granulocyte activation during hemodialysis with regional citrate anticoagulation: dissociation of complement activation and neutropenia from neutrophil degranulation. J Am Soc Nephrol 7:234–241
Gritters M, Grooteman MP, Schoorl M, Schoorl M, Bartels PC, Scheffer PG, Teerlink T, Schalkwijk CG, Spreeuwenberg M, Nubé MJ (2006) Citrate anticoagulation abolishes degranulation of polymorphonuclear cells and platelets and reduces oxidative stress during haemodialysis. Nephrol Dial Transplant 21:153–159
Faybik P, Hetz H, Mitterer G, Krenn CG, Schiefer J, Funk GC, Bacher A (2011) Regional citrate anticoagulation in patients with liver failure supported by a molecular adsorbent recirculating system. Crit Care Med 39:273–279
Balogun RA, Turgut F, Caldwell S, Abdel-Rahman EM (2011) Regional citrate anticoagulation in critically ill patients with liver and kidney failure. J Nephrol. doi:10.5301/JN.2011.8363
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Hongying, N. Efficacy and safety of regional citrate anticoagulation in critically ill patients undergoing continuous renal replacement therapy. Intensive Care Med 38, 20–28 (2012). https://doi.org/10.1007/s00134-011-2438-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2438-3