Abstract
Objective
To analyze the relationship between alcohol consumption and incident HIV infection.
Methods
Articles were identified via electronic and hand searches. Inclusion criteria were: incident HIV infection, preceding alcohol consumption, and association relating the two. The DerSimonian and Laird random effects model was used. For studies with more than one estimate of a given type, estimates were combined using the inverse variance weighted method. Publication bias was assessed using Begg’s and Egger’s tests. Heterogeneity was assessed using Q and I 2 statistics.
Results
Ten studies were included. Overall alcohol consumption (any of the three types identified) increased the risk of HIV (RR 1.98, 95% CI 1.59–2.47). Alcohol consumers were at 77% higher risk (RR 1.77, 95% CI 1.43–2.19). Those consuming alcohol prior to, or at the time of, sexual relations were at an 87% increased risk (RR 1.87, 95% CI 1.39–2.50). For binge drinkers, the risk was double that of non-binge drinkers (RR 2.20, 95% CI 1.29–3.74).
Conclusions
Alcohol consumption is associated with an increased risk of incident HIV infection. Additional research is required to further investigate a possible causal role.
Similar content being viewed by others
Introduction
At the end of 2007, globally, an estimated 33.2 million people were living with human immunodeficiency virus (HIV), 2.5 million of whom were newly infected that year (World Health Organization 2008). The disease, however, is not distributed equally among the countries of the world; indeed, the burden of disease and resultant consequences are disproportionately high in developing nations. Those nations most heavily affected have experienced a reduction in life expectancy of more than 20 years, stunted economic growth and increased household poverty (UNAIDS 2008). Although some of the most worrisome increases in new infections are now occurring in populous countries such as Indonesia, the Russian Federation, and various high-income countries, Sub-Saharan Africa continues to be the area most heavily affected by HIV, accounting for 67% of all people living with HIV and for 75% of AIDS deaths in 2007 (UNAIDS 2008).
Concomitantly, global alcohol consumption has increased in recent decades, and most of this increase has occurred in developing countries, many of which are also experiencing pronounced HIV epidemics (World Health Organization 2002). Incidentally, alcohol has often been implicated as a contributing factor for unprotected sexual behavior and subsequent HIV seroconversion, and a variety of mechanisms have been purported to underlie this alcohol-risky sex-HIV seroconversion association. It has been suggested, for example, that alcohol may have a direct physiological impact on risk behavior, leading to disinhibition (Dingle and Oei 1997) or a constriction of cognitive resources (Steele and Josephs 1990) that can in turn cause individuals to disregard relevant risk-related information when deciding whether or not to use condoms. Alternatively, the alcohol-risky sex-HIV seroconversion association may be a relatively more indirect one, in that expectations regarding alcohol consumption and condom use may in and of themselves influence individuals’ decisions to use condoms (Bryan et al. 2007; Crowe and George 1989; George and Stoner 2000; Gordon et al. 1997; LaBrie et al. 2005; Maisto et al. 2002; Murphy et al. 1998), or that individuals with certain personality types, such as those high on the dimensions of sensation seeking or sexual compulsivity, may have a disposition to engage in both high-risk sexual behavior and high-risk alcohol consumption (e.g., (Benotsch et al. 1999, 2001; Kalichman et al. 1994, 1996, 2002; Kalichman and Cain 2004; Kalichman and Rompa 1995). Finally, alcohol may have a direct biological effect on the immune system, possibly increasing the likelihood of acquiring, through risky sexual behavior, not only sexually transmitted infections (STIs) that can facilitate HIV infection, but also HIV infection itself (e.g., (Bagasra et al. 1996; Szabo 1997)).
Despite these theoretical mechanisms that have been suggested to underlie the alcohol-risky sex association, empirical support for this association is quite mixed. Although there is evidence for a significant alcohol-risky sex association when alcohol is assessed in terms of generalized or problematic use, research suggests that the association becomes attenuated when alcohol consumption is assessed specifically within the context of sexual activity (Halpern-Felsher et al. 1996; Kalichman et al. 2007a; Leigh 2002; Leigh et al. 2008; Leigh and Stall 1993; Weinhardt and Carey 2000). Similarly, regarding alcohol’s association with the incidence of STIs and HIV, although there is support for significant alcohol–STI (Cook and Clark 2005) and alcohol–HIV associations (Fisher et al. 2007), this evidence is for the most part is based on studies that assessed generalized alcohol consumption using cross-sectional methodological approaches. Because neither alcohol use prior to sexual activity nor alcohol use prior to HIV infection was typically focused on in these studies, a substantive conclusion regarding alcohol’s link to HIV incidence is difficult to make based on the available evidence.
Given these limitations, the present investigation was designed to extend prior research involving alcohol-risky sex and alcohol-risky sex-HIV seroconversion associations by conducting a meta-analysis that more clearly tested the temporal association between alcohol consumption and HIV incidence. Specifically, meta-analytic procedures were employed to examine whether alcohol use that occurred prior to HIV serconversion, including alcohol use that took place within sexual contexts, was associated with incident HIV infection.
Methods
This meta-analysis was concerned with estimating the risk of incident HIV associated with alcohol consumption, thus studies were sought which incorporated an appropriate temporal component. That is, all alcohol consumption measures had to precede HIV infection; the measure, even if taken at the time of HIV ascertainment, had to pertain to a time prior to infection ascertainment. Only newly diagnosed incident HIV infections were of interest, thus studies had to be designed to exclude prevalent HIV cases. Any direct measure of alcohol consumption was accepted, including self-reported consumption, but excluding indirect measures such as patronizing social clubs. Additionally, due to the need to quantitatively pool results, studies were required to present, or provide sufficient data for the calculation of, a measure of association (i.e., odds ratio, relative risk, or hazard ratio) between alcohol consumption and incident HIV infection.
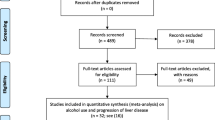
Figure 1 summarizes the process for selecting articles included in the meta-analysis. Articles included were found via a search of the following indices and sources: Medline, via OVID and Pubmed (1950 to May 2008), CINAHL (1982 to May 2008), and EMBASE (1980 to May 2008). The databases were searched for reports with keywords alcohol or ethanol, incidence or incident or risk or seroincidence or seroconvert*, and with title words HIV* or human immunodeficiency virus or STI or STIs or sexually transmitted infection* or STD or STDs or sexually transmitted disease*. Animal studies and commentaries, editorials, letters and review articles were excluded. No language restriction was applied.
Data abstracted included descriptors of the study design in addition to the measures of association. The measures of effect abstracted were hazard ratios, odds ratios, and relative risks. Where some intermediate consumption group was used as the reference, the RRs were reformulated to make abstainers the reference group. Where measures of association were not specifically presented, but sufficient information was available, they were calculated. Adjusted estimates were preferred over crude ones, though crude were accepted.
Three separate types of alcohol consumption risks were found; those pertaining to consumption, binge consumption, and consumption prior to, or at the time of, sexual relations. Both type-specific and overall analyses were conducted. Three sensitivity analyses were completed. One sensitivity analysis was performed for the overall combined category only, comparing studies arising from developed and developing nations. For the second analysis, we stratified the studies by sex and calculated separate risk estimates for women and men. The third sensitivity analysis included only men and we compared risks in studies with MSM samples and those using samples of other men. All analyses were conducted using Stata version 10 software (StataCorp 2008). Meta-analysis was conducted using the DerSimonian and Laird random effects model using the metan command. Three articles had more than one estimate of a given type (Koblin et al. 2006; Read et al. 2007; Zablotska et al. 2006). For example, Read et al. 2007 had estimates for three separate levels of alcohol consumption prior to sex. Thus, for each of those studies for which more than one estimate of a given type was available, the estimates were combined prior to analysis using the inverse variance weighted method to obtain one estimate of a given type per study. Publication bias was assessed using the Begg’s test (Begg and Mazumdar 1994) and Egger’s test (Egger et al. 1997). Heterogeneity was assessed using the Q-statistic and the I 2 statistic. However, random effects were used throughout in order to be conservative.
Results
The electronic search strategy resulted in 856 hits after the removal of duplicates. The abstracts, or complete publication if abstracts were unavailable, were reviewed and excluded if they contained no indication of a measure of association between alcohol consumption and risk of incident HIV (n = 792) or the measure of association was cross-sectional (n = 53). One article could not be acquired bringing the number of articles to 10. The references of these articles were hand-searched for additional publications. Twenty-seven articles were identified by this hand search of which five remained after applying the same exclusion criteria described above (Fig. 1). Combining the database and hand searches, 15 articles were identified for data abstraction. However, two were excluded because they were duplicate publications from a given study; in cases where more than one publication was generated from a given study, the most comprehensive report, and not necessarily the most recently published, was included in the meta-analysis. One article was excluded because the association between alcohol and HIV risk was not reported as a measure of association and insufficient data were provided for the authors to make this calculation (Kippax et al. 1998). One type of estimate from one article (Plankey et al. 2007), and one entire article (Wang et al. 2005) were excluded because the measures of association for alcohol consumption used a non-abstaining reference group. One article was excluded because the alcohol consumption definition pertained to any alcohol consumption during the teenage years, which the authors felt was too general and unlikely to pertain to risk for acquiring HIV in this adult sample (Krantz et al. 2002). Thus, the final analysis sample consisted of ten articles.
Characteristics of the ten articles included in the analysis are presented in Table 1 (Celentano et al. 1996; Chesney et al. 1998; Figueroa et al. 1997; Kapiga et al. 1998; Koblin et al. 2006; Nopkesorn et al. 1998; Page-Shafer et al. 1997; Plankey et al. 2007; Read et al. 2007; Zablotska et al. 2006). Because three articles presented two different types of alcohol consumption categories, the ten articles provided 13 estimates (Celentano et al. 1996; Koblin et al. 2006; Read et al. 2007). Eight articles included only men, one included only women, and one both men and women (separately), thus sex-specific analyses were only conducted as sensitivity analyses. Eight articles described prospective cohorts, one a nested case–control, and one a case–control study. Adjustment for confounders varied, and nine of the 13 estimates were crude. Incident HIV infection in persons formerly known to be HIV negative was ascertained, in nine out of ten articles, by enzyme linked immunosorbent assay (ELISA) confirmed with a western blot. In the 10th study, incident HIV infection was determined via a registry (Read et al. 2007). Finally, half the articles report on studies that took place in developing nations: Jamaica, Tanzania, Thailand (×2), and Uganda.
Both the Egger’s and Begg’s tests showed no publication bias (P = 0.526 and P = 0.067, respectively). Among the 13 estimates, there was significant heterogeneity (P < 0.001). Among the three consumption type-specific estimates, only the binge estimates displayed significant heterogeneity (P < 0.001).
The forest plot in Fig. 2 depicts the estimates from the 13 articles, the consumption type-specific pooled estimates, and the overall pooled estimate. Random effects analysis of the association between overall alcohol consumption (any of the three types of alcohol consumption) and incident HIV infection shows that those who consume alcohol have a significantly higher risk of becoming HIV positive (pooled RR 1.98, 95% CI 1.59–2.47). For each of the consumption type-specific analysis, the risk of HIV infection was also greater among consumers. Those who consumed any alcohol were at 77% higher risk of acquiring HIV than those who did not consume alcohol at all (pooled RR 1.77, 95% CI 1.43–2.19). Those consuming alcohol prior to, or at the time of, sexual relations were at an 87% increased risk (pooled RR 1.87, 95% CI 1.39–2.50). For those consuming alcohol in binges, the risk of HIV infection was over double that of non-binge drinkers (pooled RR 2.20, 95% CI 1.29–3.74).
Table 2 reports the results of the sensitivity analyses. The first sensitivity analysis showed similar results in association between overall alcohol consumption (any of the three types of alcohol consumption) and incident HIV infection found in developed nations (pooled RR 1.97, 95% CI 1.37–2.81) and developing nations (pooled RR 1.91, 95% CI 1.55–2.35). Secondly, the effect of alcohol on the risk for HIV was similar among the non-MSM population (pooled RR 2.08, 95% CI 1.46–2.98) and the MSM population (pooled RR 1.92, 95% CI 1.30–2.83) and the P value for the formal test of interaction between the MSM and non-MSM populations was not significant (P = 0.75), implying that the chance could not be ruled out as underlying the slight differences in impact of alcohol on the risk of HIV in the MSM and the non-MSM populations. Finally, we also observed no significant differences in risk by sex (P interaction = 0.83) or by developing versus developed nations (P interaction = 0.88).
Discussion
The present meta-analysis lends support to the hypothesis that alcohol consumption is associated with an increased risk of acquiring HIV infection.
This finding is consistent with the Fisher meta-analysis which explicitly limited its focus to studies taking place in Africa (Fisher et al. 2007). Indeed, although we restricted our selection criteria to incident HIV measures, and the Fisher analysis did not, we found similar measures of effect (Fisher ORunadjusted of 1.70, 95% CI 1.45–1.99; ORadjusted 1.57, 95% CI 1.42–1.72; Baliunas OR 1.77, 95% CI 1.43–2.19). Remarkably, even though studies selected for inclusion into our meta-analyses differed widely with variations by study type, geography, population and exposure measurement, there was no significant heterogeneity in effect size in the meta-analysis for drinker versus non-drinker or in the analysis pertaining to a drinking prior to sexual activity. Additionally, our sensitivity analyses showed no differences based on sex, sexual practices or region. Each of the alcohol consumption categories was positively associated with risk of incident HIV. Also, lending consistency to the overall conclusion is the finding that binge drinking has a larger effect size. This hints at a gradient—more alcohol, more risk. A recent large cohort study corroborates these results. The authors found an overall adjusted odds ratio of 2.10 for any kind of drinking (95% CI 1.29–3.42) in a cohort of 1,050 high-risk African women. Greater involvement of alcohol, as defined by recency, quantity or frequency consumed, was associated with greater risk. Problem drinkers as identified by two positive answers on a screening instrument for alcohol dependence had a higher risk (OR 2.43, 95% CI 1.45–4.06) than non-problem drinkers (OR 1.79, 95% CI 1.06–3.04) (Fisher et al. 2008).
There are several possible explanations for the observed association between alcohol consumption and HIV risk. Alcohol consumption may exert a true effect on risk of HIV infection via some effect on the immune system, either local or general, or via altered behavior including partner selection and condom (non) use. Alternatively, the observed association may not reflect a causal effect, but a common antecedent confounder. Put this way, the implication is that alcohol consumption is a marker for some personality trait which causes both alcohol consumption and the propensity to engage in risky sexual behaviors. There is also the role of prior expectations or beliefs about alcohol to consider; it may be one’s belief that alcohol leads to behavior inhibition, and not the alcohol per se, that leads to HIV risk. In this way, alcohol expectancies may confound the relationship between consumption and HIV risk.
There are several limitations to the present analysis which must be acknowledged. For practical purposes, the search strategy required the presence of the keywords alcohol or ethanol. Thus, there may exist additional relevant reports that included alcohol consumption as a covariate and for which sufficient information exists to calculate measures of association. One might suspect that studies which found a significant association would be more likely to include the term alcohol in their abstracts or keywords, would be more likely to have been identified in our search strategy, and hence may have biased the findings upwards. However, no evidence of publication bias was detected, which provides some assurance against this possibility. While no publication bias was detected, there are a number of other types of bias that may affect the results. All studies that met inclusion criteria were included with no exclusions due to study quality. This choice was made due to the small number of studies identified and the adjuvant recognition that a more strict approach would not help public health practitioners struggling to make recommendations based on the evidence that currently exists. Case ascertainment was rigorous in all studies, but exposure ascertainment in alcohol research is less straightforward, as evidenced by the variety of consumption measures reported. While most studies were prospective and thus recall bias is not implicated (which would require a differential rate of reported among affected and unaffected individuals), there may nonetheless have been some exposure misclassification due to desirability bias. However, any resulting misclassification is likely to be non-differential, and thus would lead to an attenuation of any effect. Alcohol exposure preceded HIV seroconversion in all cases. However, the amount of time between exposure and outcome varied between studies and participants. Exposure was generally ascertained upon study entry or subsequent follow-up interview, and outcome was ascertained on regular follow-up or study completion. What the precise etiologically relevant time period for alcohol consumption might be, and whether participants consumed during that precise time, cannot be determined from our analysis.
This meta-analysis is insufficient to address which, if any, of the above-described potential explanations for the association between alcohol exposure and HIV are at work. Indeed, although the temporal causal criteria is satisfied (by design), and the results suggest some consistency of evidence, the evidence on the whole is insufficient to conclude a causal link. At most, one might state that the evidence is suggestive and bears further research.
This meta-analysis is the first to examine the association between alcohol consumption and incident HIV infection, and as such, is a significant contribution to the existing literature. However, more and better research is needed. In particular, to adequately address this important question, several methodological improvements will need to be made: better and consistent measures of alcohol consumption including objective measures; prospective studies that allow for the path analyses of the various pathways; more studies among female populations to allow for sex-specific meta-analysis.
With regard to public health practice, the consistent and relatively strong association between alcohol consumption and HIV incidence, together with the high risk of HIV infection and relatively high prevalence of heavy drinking occasions in Sub-Saharan Africa (Rehm et al. 2009) should lead to the inclusion of alcohol-specific interventions into HIV risk reduction packages. Such a strategy has already been introduced by Kalichman et al. (2007b, 2008), albeit with mixed results. Thus, if proven short but effective alcohol interventions such as Brief Interventions (Room et al. 2005) are included in HIV risk reduction packages, it should be done with experimental variation in order to be able to isolate any potential effects of the alcohol interventions. After all, this strategy would not only identify the most effective interventions, it would also provide a mechanism by which to further explore the causal association.
References
Bagasra O, Bachman SE, Jew L, Tawadros R, Cater J, Boden G, Ryan I, Pomerantz RJ (1996) Increased human immunodeficiency virus type 1 replication in human peripheral blood mononuclear cells induced by ethanol: potential immunopathogenic mechanisms. J Infect Dis 173:550–558
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Benotsch EG, Kalichman SC, Kelly JA (1999) Sexual compulsivity and substance use in HIV-seropositive men who have sex with men: prevalence and predictors of high-risk behaviors. Addict Behav 24:857–868
Benotsch EG, Kalichman SC, Pinkerton SD (2001) Sexual compulsivity in HIV-positive men and women: prevalence, predictors, and consequences of high-risk behaviors. Sexual Addict Compuls 8:83–99
Bryan A, Ray LA, Cooper ML (2007) Alcohol use and protective sexual behaviors among high-risk adolescents. J Stud Alcohol Drugs 68:327–335
Celentano DD, Nelson KE, Suprasert S, Eiumtrakul S, Tulvatana S, Kuntolbutra S, Akarasewi P, Matanasarawoot A, Wright NH, Sirisopana N (1996) Risk factors for HIV-1 seroconversion among young men in northern Thailand. JAMA 275:122–127
Chesney MA, Barrett DC, Stall R (1998) Histories of substance use and risk behavior: precursors to HIV seroconversion in homosexual men. Am J Public Health 88:113–116
Cook RL, Clark DB (2005) Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sex Transm Dis 32:156–164
Crowe LC, George WH (1989) Alcohol and human sexuality: review and integration. Psychol Bull 105:374–386
Dingle GA, Oei TP (1997) Is alcohol a cofactor of HIV and AIDS? Evidence from immunological and behavioral studies. Psychol Bull 122:56–71
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315:629–634
Figueroa JP, Ward E, Morris J, Brathwaite AR, Peruga A, Blattner W, Vermund SH, Hayes R (1997) Incidence of HIV and HTLV-1 infection among sexually transmitted disease clinic attenders in Jamaica. J Acquir Immune Defic Syndr Hum Retrovirol 15:232–237
Fisher JC, Bang H, Kapiga SH (2007) The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis 34:856–863
Fisher JC, Cook PA, Sam NE, Kapiga SH (2008) Patterns of alcohol use, problem drinking, and HIV infection among high-risk African women. Sex Transm Dis 35:537–544
George WH, Stoner SA (2000) Understanding acute alcohol effects on sexual behavior. Annu Rev Sex Res 11:92–124
Gordon CM, Carey MP, Carey KB (1997) Effects of a drinking event on behavioral skills and condom attitudes in men: implications for HIV risk from a controlled experiment. Health Psychol 16:490–495
Halpern-Felsher BL, Millstein SG, Ellen JM (1996) Relationship of alcohol use and risky sexual behavior: a review and analysis of findings. J Adolesc Health 19:331–336
Kalichman SC, Cain D (2004) The relationship between indicators of sexual compulsivity and high risk sexual practices among men and women receiving services from a sexually transmitted infection clinic. J Sex Res 41:235–241
Kalichman SC, Rompa D (1995) Sexual sensation seeking and Sexual Compulsivity Scales: reliability, validity, and predicting HIV risk behavior. J Pers Assess 65:586–601
Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA (1994) Sexual sensation seeking: scale development and predicting AIDS-risk behavior among homosexually active men. J Pers Assess 62:385–397
Kalichman SC, Heckman T, Kelly JA (1996) Sensation seeking as an explanation for the association between substance use and HIV-related risky sexual behavior. Arch Sex Behav 25:141–154
Kalichman SC, Weinhardt L, DiFonzo K, Austin J, Luke W (2002) Sensation seeking and alcohol use as markers of sexual transmission risk behavior in HIV-positive men. Ann Behav Med 24:229–235
Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S (2007a) Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci 8:141–151
Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K (2007b) HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. J Acquir Immune Defic Syndr 44:594–600
Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, Jooste S (2008) Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Ann Behav Med 36:270–279
Kapiga SH, Lyamuya EF, Lwihula GK, Hunter DJ (1998) The incidence of HIV infection among women using family planning methods in Dar es Salaam, Tanzania. AIDS 12(1):75–84
Kippax S, Campbell D, Van de Ven P, Crawford J, Prestage G, Knox S, Culpin A, Kaldor J, Kinder P (1998) Cultures of sexual adventurism as markers of HIV seroconversion: a case control study in a cohort of Sydney gay men. AIDS Care 10(6):677–688
Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Barresi PJ, Coates TJ, Chesney MA, Buchbinder S (2006) Risk factors for HIV infection among men who have sex with men. AIDS 20(5):731–739
Krantz SR, Lynch DA, Russell JM (2002) Gender-specific profiles of self-reported adolescent HIV risk behaviors. J Assoc Nurses AIDS Care 13(6):25–33
LaBrie J, Earleywine M, Schiffman J, Pedersen E, Marriot C (2005) Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. J Sex Res 42:259–266
Leigh BC (2002) Alcohol and condom use: a meta-analysis of event-level studies. Sex Transm Dis 29:476–482
Leigh BC, Stall R (1993) Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol 48:1035–1045
Leigh BC, Morrison DM, Hoppe MJ, Beadnell B, Gillmore MR (2008) Retrospective assessment of the association between drinking and condom use. J Stud Alcohol Drugs 69:773–776
Maisto SA, Carey MP, Carey KB, Gordon CM (2002) The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. J Stud Alcohol 63:476–485
Murphy ST, Monahan J, Miller LC (1998) Inference under the influence: the impact of alcohol and inhibition conflict on women’s sexual decision making. Pers Soc Psychol Bull 24:517–528
Nopkesorn T, Mock PA, Mastro TD, Sangkharomya S, Sweat M, Limpakarnjanarat K, Laosakkitiboran J, Young NL, Morse SA, Schmid S, Weniger BG (1998) HIV-1 subtype E incidence and sexually transmitted diseases in a cohort of military conscripts in northern Thailand. J Acquir Immune Defic Syndr Hum Retrovirol 18(4):372–379
Page-Shafer K, Veugelers PJ, Moss AR, Strathdee S, Kaldor JM, van Griensven GJ (1997) Sexual risk behavior and risk factors for HIV-1 seroconversion in homosexual men participating in the Tricontinental Seroconverter Study, 1982–1994. Am J Epidemiol 146:531–542
Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, Jacobson LP (2007) The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr 45(1):85–92
Read TR, Hocking J, Sinnott V, Hellard M (2007) Risk factors for incident HIV infection in men having sex with men: a case-control study. Sex Health 4(1):35–39
Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J (2009) Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 373:2223–2233
Room R, Babor T, Rehm J (2005) Alcohol and public health. Lancet 365:519–530
StataCorp (2008) Stata Statistical Software: Release 10.1. Stata Corporation, College Station
Steele CM, Josephs RA (1990) Alcohol myopia. Its prized and dangerous effects. Am Psychol 45:921–933
Szabo G (1997) Alcohol’s contribution to compromised immunity. Alcohol Health Res World 21:30–41
UNAIDS (2008) 2008 Report on the global AIDS epidemic. UNAIDS, Geneva
Wang C, Vlahov D, Galai N, Cole SR, Bareta J, Pollini R, Mehta SH, Nelson KE, Galea S (2005) The effect of HIV infection on overdose mortality. AIDS 19:935–942
Weinhardt LS, Carey MP (2000) Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res 11:125–157
World Health Organization (2002) World Health Report 2002. WHO, Geneva
World Health Organization (2008) Towards universal access : scaling up priority HIV/AIDS interventions in the health sector : progress report 2008. World Health Organization, Geneva
Zablotska IB, Gray RH, Serwadda D, Nalugoda F, Kigozi G, Sewankambo N, Lutalo T, Mangen FW, Wawer M (2006) Alcohol use before sex and HIV acquisition: a longitudinal study in Rakai, Uganda. AIDS 20:1191–1196
Acknowledgments
We thank the attendees of the Alcohol and Infectious Diseases Technical meeting held in Cape Town, South Africa in July 2008 and hosted by the South African Medical Research Council in collaboration with the World Health Organization. The research work was funded by the South African Medical Research Council (MRC) through a grant received from the US President’s Emergency Fund for AIDS Relief (PEPFAR) through the US Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baliunas, D., Rehm, J., Irving, H. et al. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health 55, 159–166 (2010). https://doi.org/10.1007/s00038-009-0095-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-009-0095-x