Abstract
Objective: To compare the effect of macrolide and fluoroquinolone antibacterials on the onset of ventricular arrhythmia and cardiac arrest using three different observational designs.
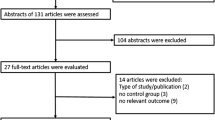
Methods: A population-based case-control study was performed by linking automated databases from the Varese Province of Italy. Cases were all subjects who experienced ventricular arrhythmia or cardiac arrest from July 1998 to December 2003. For each case, up to ten controls were randomly selected after matching for sex, age, practitioner and date of arrhythmia onset. The use of macrolides and fluoroquinolones during two time windows denoted as recent and referent intervals was ascertained. Odds ratios were estimated using case-control, case-crossover and case-time-control approaches.
Results: 1275 cases and 9189 controls met the inclusion criteria. Adjusted odds ratios (and corresponding 95% CIs) associated with recent exposure to macrolides were 2.13 (1.34, 3.39), 1.70 (0.88, 3.26) and 1.62 (0.78, 3.34) by using case-control, case-crossover and case-time-control designs, respectively. The corresponding estimates for fluoroquinolones were 3.58 (2.51, 5.12), 1.98 (1.19, 3.29) and 1.59 (0.88, 2.87), respectively.
Conclusions: Three observational study designs each using entirely different sets of controls consistently showed that recent use of macrolide and fluoro-quinolone antibacterials may be associated with increased risk of ventricular arrhythmia and cardiac arrest.


Similar content being viewed by others
References
Viskin S, Justo D, Halkin A, et al. Long QT syndrome caused by noncardiac drugs. Progr Cardiovasc Dis 2002; 45: 415–27
De Ponti F, Poluzzi E, Cavalli A, et al. Safety of non-arrhythmic drugs that prolong the QT interval or induce torsade de pointes. Drug Saf 2002; 25: 263–86
Clark DW, Layton D, Wilton LV, et al. Profiles of hepatic and dysrhythmic cardiovascular events following use of fluoroquinolone antibacterials: experience from large cohorts from the Drug Safety Research Unit Prescription-Event Monitoring database. Drug Saf 2001; 24: 1143–54
De Bruin ML, Hoes AW, Leufkens HG. QTc-prolonging drugs and hospitalizations for cardiac arrhythmias. Am J Cardiol 2003; 91: 59–62
Ray WA, Murray KT, Meredith S, et al. Oral erythromycin and the risk of sudden death from cardiac causes. N Engl J Med 2004; 351: 1089–96
Corrao G, Botteri E, Bagnardi V, et al. Generating signals of drug-adverse effects from prescription databases and application to the risk of arrhythmia associated with antibacterials. Pharmacoepidemiol Drug Saf 2005; 14: 31–40
Bagnardi V, Botteri E, Corrao G. Empirical-Bayes adjustment for multiple results in post-marketing drug safety surveillance with application to antibacterials and arrhythmia. J Clin Epidemiol 2006; 59: 1162–8
Corrao G, Botteri E, Bertù L, et al. Exploring the effect of transient exposure on the risk of acute events by means of time-window designs: an application to fluoroquinolone antibacterials and arrhythmia. Pharmacoepidemiol Drug Saf 2006; 15: 31–7
Suissa S. Pharmacoepidemiology overview. In: Gail MH, Benichou J, editors. Encyclopedia of epidemiologic methods. New York: John Wiley & Sons, 2000: 702–12
Smeeth L, Donnan PT, Cook DG. The use of primary care databases: case-control and case-only designs. Fam Pract 2006; 23: 597–604
Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 1991; 113: 144–53
Suissa S. The case-time-control design. Epidemiology 1995; 6: 248–53
Hernandez-Diaz S, Hernan MA, Meyer K, et al. Case-crossover and case-time-control designs in birth defects epidemiology. Am J Epidemiol 2003; 158: 385–91
Meyer KA, Williams P, Hernandez-Diaz S, et al. Smoking and the risk of oral clefts: exploring the impact of study designs. Epidemiology 2004; 15: 671–8
Schneider MF, Gange SJ, Margolick JB, et al. Application of case-crossover and case-time-control study designs in analyses of time-varying predictors of T-cell homeostasis failure. Ann Epidemiol 2005; 15: 137–44
Corrao G, Zambon A, Faini S, et al. Short-acting inhaled beta-2-agonists increased the mortality from chronic obstructive pulmonary disease in observational designs. J Clin Epidemiol 2005; 58: 92–7
Staffa JA, Jones JK, Gable CB, et al. Risk of selected serious cardiac events among new users of antihistamines. Clin Ther 1995; 17: 1062–77
Singh SN, Patrick J. Antiarrhythmic drugs. Curr Treat Options Cardiovasc Med 2004; 6: 357–64
Breslow NE, Day NE. Statistical methods in cancer research. Volume I: the analysis of case-control studies. IARC Scientific Publications No. 32. Lyon: International Agency for Research on Cancer, 1980
Leufkens HG, Urquhart J. Variability in patterns of drug usage. J Pharm Pharmacol 1994; 46: 433–7
Greenland S, Gustafson P. Accounting for independent nondifferential misclassification does not increase certainty that an observed association is in the correct direction. Am J Epidemiol 2006; 164(1): 63–8
Shaffer D, Singer S, Korvick J, et al. Concomitant risk factors in reports of torsades de pointes associated with macrolide use: review of the United States Food and Drug Administration Adverse Event Reporting System. Clin Infect Dis 2002; 35: 197–200
Matsunaga N, Oki Y, Prigollini A. A case of QT-interval prolongation precipitated by azithromycin. N Z Med J 2003; 116(1185): U666
Smeeth L, Thomas SL, Hall AJ, et al. Risk of myocardial infarction and stroke after acute infection or vaccination.
Salas M, Hofman A, Strieker BHC. Confounding by indication: an example of variation in the use of epidemiologic terminology. Am J Epidemiol 1999; 149: 981–3
Zabel M, Hohnloser SH, Behrens S, et al. Electrophysiologic features of torsades de pointes: insights from a new isolated rabbit heart model. J Cardiovasc Electrophysiol 1997; 8: 1148–58
Antzelevitch C. Cellular basis and mechanism underlying normal and abnormal myocardial repolarization and arrhythmogenesis. Ann Med 2004; 36 Suppl. 1: 5–14
Greenland S. Confounding and exposure trend in casecrossover and case-time-control designs. Epidemiology 1996; 7: 321–7
Suissa S. The case-time-control design: further assumptions and conditions. Epidemiology 1998; 9: 441–5
Acknowledgements
Support for this study was received from the M.I.U.R. (Italian Ministry of the Instruction, University and Research) grants (“Fondo d’Ateneo per la Ricerca” portion, year 2005, and PRIN portion, protocol n∘ 2005068001, year 2005). The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zambon, A., Polo, H., Contiero, P. et al. Effect of Macrolide and Fluoroquinolone Antibacterials on the Risk of Ventricular Arrhythmia and Cardiac Arrest. Drug-Safety 32, 159–167 (2009). https://doi.org/10.2165/00002018-200932020-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200932020-00008